Clinicians Corner | From Feels to Force Plates
Why Dynamometry is a MSK Clinician’s Best Friend
This is a no-paywall blog post with insights I believe are valuable. If you find it useful, subscribe to my Substack for more in-depth content, exclusive case studies, and clinical insights.
Your support helps me continue sharing everything I’ve learned in the clinic with the world.
☕ Prefer a one-off thank you? Buy Me a Coffee.
This post is a guide only and should not be taken as medical advice. It does not replace assessment and recommendations from a registered and regulated healthcare professional.
Recently, I was flabbergasted, gobsmacked and bamboozled when I saw some prominent Physiotherapists online poo-poo Dynamometry.
“It’s Death by Data”
“Does all that data really guide rehab decisions?”
“I don’t need it ergo it’s not needed” said the world-renowned experts, who are outstanding in their fields.
What I noticed however, was these experts are the sort who mostly see crop circles, instead of crops.
These experts are seeing the outliers for 2nd opinion work where dynamometry might not be as relevant as the local Sports Physio clinic with weekend warriors and athletes.
Perhaps cognitive behaviour therapy is more appropriate than isokinetic dynamometry for that chronic back. Or maybe that patient just needs to get back in the gym and push through that 1-2/10 pain they’ve been avoiding for their chronic patella tendon– don’t need dynamometry for that, right?
In fairness, after some online outrage (as happens on days that end in -y) one of those experts later stated that it’s probably useful for those rehabbing patients post-ACLR (for example), where we use it to make smart rehab decisions as part of ‘Criteria Based Rehab’.
But lets' hold our horses.... what in the cotton-picking, clinical-confounding balderdash is: DYNAMOMETRY
Dynamometry
Dyna- as a prefix, usually refers to ‘power.’
Therefore Dyna-mom-etry appears to translate to
“The Measurement of how Powerful your Mom is.”
But in our line of work, it is: The Measurement of Force.
Not ‘Strength’, but ‘force’.
In particular, the Ability to Produce Force (force production).
Our ability to push or pull a thing, whether that thing be static (aka ‘iso,’ not moving) or moving (aka ‘kinetic’).
Whether that thing be a device, another human, a wall, or the ground (which is usually static, unless you’re in Parkfield, California).

However, it is the use of Dynamometry as a ‘how happy is that joint to do its job’ tool where it best enters the Clinical Reasoning part of the mushy-jelly thing inside your head.
How does “strength” fit into this?
You want the most amazing little formula for how to work out the difference, see Ian Gatt’s article in Msk Mag:
“Force = Strength – Pain”
Oh, my goodness, I need a moment, I just read it out loud again and need to settle down from my giddiness – here watch this whilst I compose myself
……Ok I’m back
“Force = Strength – Pain”
Sometimes weak and painful joints just need to get pain under control, then guess what happens when there’s less pain?
Here, let me solve this complex equation:
There you go folks – when there is less Pain, Force Production increases.
We don’t even have to call them “weak” and give them “strength exercises”.
So, Luke…
yes YOU Luke…
don’t look around I’m talking about you
Don’t use the word “strength” when talking about dynamometry…. instead:
Yes.
Use “Force” (or “force production”).
Types of Tests
Earlier, before the gratuitous and deeply nerdy Stars Wars reference and the Good Will Huntingesque Maths Equation, I mentioned the following words ‘iso’ and ‘kinetic.’
Isokinetic Dynamometry (IKD) is the Gold Standard for assessing strength force… and it gets ACL and Sports Medicine Research nerds extremely excited.
I won’t do a deep dive into this type of dynamometry because not many of us have the deep pockets needed to get this deep into assessment.
Put simply: this device moves the patient’s limb (locked in a pad) at a set speed (usually around 60-180 degrees per second) while the patient pushes against the pad. It finds out how forceful patients are through the range of the joint (or their torque), at different speeds which usually line up with the requirements of their sport.
If you can’t afford an IKD, you can crack on with the most common form of Dynamometry in good clinics around the world:
Isometric testing
The measure (-metric) of how hard you produce force against a static (iso-) thing.
Examples of Isometric testing:
Squatting on force plates = a dynamic isometric task (you move, it doesn’t).
Pushing out into external rotation with your shoulder against a handheld dynamometer (HHD) = a static isometric task (nothing moves).
Sitting on a bench and kicking your leg out into extension, against a strap holding your ankle back, attached to an Inline Dynamometer which is fixed underneath you (nothing moves).
A HHD is a somewhat expensive but useful and hopefully rugged yet mobile device with load cells and other gadgetry in it. Essentially, it’s a very expensive digital set of bathroom scales – these days usually with a Bluetooth connection to a Mobile Device or Tablet you can show off in front of your patients – hopefully making you appear smarter in the process.
HHDs typically measure push forces.
Force plates are heavy and rugged metal plates on the ground with thousands of load cells in them – cost a little bit more than HHDs, but they’re very useful.
Inline dynamometers measure pull forces.
Some HHDs can measure both pull and push forces.
These pull-dynamometers are very useful for assessing strong muscles - muscles such as Titanus Quadzilla a lesser known but obviously massive muscle in most road cyclists.
Inline dynamometry has even been shown to be reliable and a valid substitute for IKD in a 2024 study by Norris Et. Al. (1), which for the cost of one of these pull-dynamometers, compared to an IKD, is a bit of a relief to be honest.

In most clinics, with the above tools, we usually conduct a ‘maximum isometric test,’ where we instruct the patient (after some warmups) to “push as hard and as fast as you can and hold it for 3 seconds, ready? Set? Go!
Push! Push! Push! Push! and stop” (and repeat twice more for 3 reps).
Pedestrians walking past have confused us for a different type of healthcare clinic, we don’t deliver babies, but we do deliver reliable results that guide good rehab decisions.
Speaking of maternity wards:
Quick Tip for Instant Credibility™:
If you want a knowing head-nod from the elite sports physio crowd, always talk in ‘Newtons’ instead of kilos of force.
Doesn’t matter if the conversion is basic math—drop ‘Newtons’ into a sentence, and you’ll immediately level up in the eyes of the performance-nerds in the room.
Talking about their new car? Talk Newtons.
If they had a baby? Forget pounds—ask how many Newtons their missus generated during delivery, and whether the Rate of Force Development met the externalising demands. 🚀
Force Plates as the Discharge Gatekeeper
Every good clinician has a few ‘just-in-case-we’re-missing-something-tests’ up their sleeve before giving a patient the all-clear. Because let’s face it—rehab can look great on paper, but the body can still hide its dirty little secrets.
One such test? The Countermovement Jump (CMJ): Science for Sport Link
The CMJ is a proven proxy for athletic demands, particularly general strength, linear speed, and change of direction ability. When combined with limb symmetry index (% of left vs right), it helps sniff out hidden strength imbalances and lingering injury risk (2).
And here’s the best part—it’s dead simple. With both visual analysis (hello, slow-mo phone video) and hard objective data from the hard (hopefully soft) landings on the force plate(s), you’ll quickly see if an athlete is cheating their way through force production and absorption.
If that checks out, take it up a notch—enter the Countermovement Hop (CMH). Same concept, higher demands, more single-leg exposure.
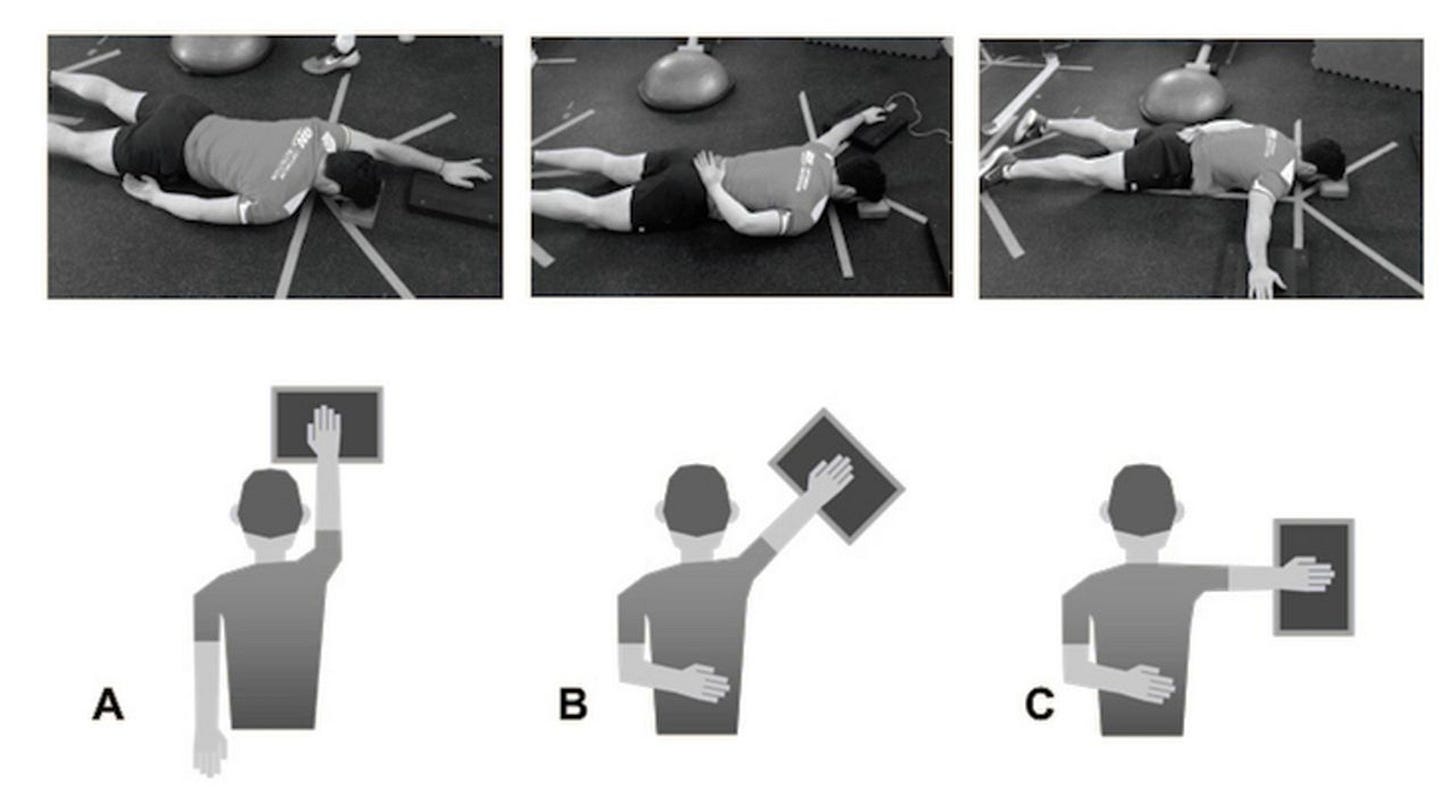
For repetitive overhead or contact athletes with shoulder injuries, the ASH/AST Shoulder Tests in the T/Y/I (90°/135°/180°) positions are gold. They measure the shoulder's ability to stabilize under load in various overhead positions—because pressing a dumbbell isn’t the same as taking a hit (2).
Are you still Manually Testing Muscles – with your hands?
“But I can feel the force.”
No. No you can’t, Luke, at least, not accurately (3).
But I believe that you think you can feel the force. You’re a Jedi Clinician who uses Manual Muscle Testing (MMT).
Manual Muscle Testing is feeling the force, with your hand, and assigning a number (out of 5) for how much force there is, here’s a MMT table in all its glory:
Ok I get it, I hear you: “please move on, we’re getting flashbacks to uni days.”
Here’s a more exciting version, just for you….Luke.
Even 30 years ago, studies were saying manual muscle testing is very subjective, and much less objective and reliable than HHD (4). For those Clinicians who are less than 70kg in weight, good luck testing the knee extension forces of my footballers with your hands. You’d better buckle up, or you’ll be their next field goal.
That’s the thing—Manual Muscle Testing (MMT) without a Handheld Dynamometer (HHD) has its place. If you’re working in neuro-rehab with stroke populations where patients aren’t expected to yeet* you across the clinic, it’s fine.
But for active populations? Hard nope.
*’Yeet’ is a technical term for unexpectedly launching an underprepared clinician across the room with unmeasured but undeniably excessive force.
A systematic review by Bohannon (2011) on the Reliability of Manual Muscle Testing found that MMT’s reliability is… well, not great (4).
Turns out, it often hinges on how optimistic (or generous) the tester is feeling that day. Sure, test-retest reliability is decent, but inter-rater reliability? About as consistent as a toddler’s bedtime routine (3).
If patients are going to go Ballistic, get a HHD.
Ooooo a Top Gun reference…. I’m triggered.
PLEASE PLAY THE CLIP BELOW whilst you read the next bit of the blog….
Just trust me…. you’ll thank me soon
Did you open it…
turn it up…….
ok perfect…... I’m gonna continue…
Where were we?… oh yes!
Yes, dynamometers are expensive, but if you think cash gets in the way of getting solid objective measures, and you’d rather gamble on your biased Manual Muscle Test feelings helping you with your patient’s healthcare…. well then:
I think your Bias is Writing Cheques Their Body Can’t Cash.
You may now discontinue the YouTube clip.
I thank you. Your workmates thank you.
So please, ditch the MMT, invest in Dynamometry….
Unless of course you are a Jedi….
Force, Feels, and Foundations: What Dynamometry Actually Measures
We use dynamometry to measure:
Ability: Can the patient move themselves through their world—or their world around them—the way they want to?
Capacity: Do they have enough physical reserves to handle what life (or their sport) throws at them?
Resilience: Are we building them a House of Bricks on solid foundations or are we gambling on guesswork (or worse, clinician bias), leaving them with a House of Straw?
Readiness = Ability + capacity + resilience, but this also includes considering the person attached to the rehabbed body part: The Human Being—complete with its mushy jelly-brain full of fears, thoughts, and feelings (Yuck! Emotions!). Even if the patient shows ✅ Full ROM and ✅ Great isolated strength, the force plate data might still say, "No thanks, not today."
Psychological readiness is essential—there’s a significant re-injury risk without it (5). Thankfully, there are excellent questionnaires (e.g., ACL RTS Questionnaire) that help capture this. But if you somehow miss capturing a patient’s readiness, the performance data from a CMJ or CMH just might give it away.
Case Studies – When Dynamometry Changed the Game
Let me tell you about Wally the Winger – he runs fast.
Wally the Winger - Football
Wally met me after a recent left hamstring strain, reporting a history of recurring left hamstring strains. His S&C and coach asked, “why does this keep happening?”
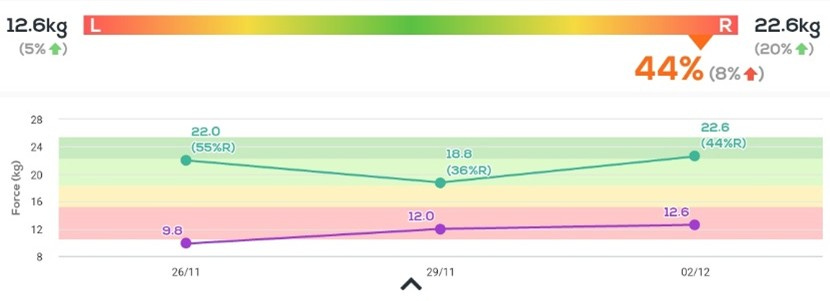
I assessed his knee flexion force production:

Yep. Left was ouchy.
We backed off training, we did some sub-pain running, we did some hip-dominant and knee-dominant knee flexion resistance training.
He got better over time.
Then guess what happened?
He wasn’t ouchy anymore. He was pain-free, but he was weak.
He had:
1. History of recurrent strains
2. Pain-free knee flexion after a few weeks but significantly less peak force than the other side
And….
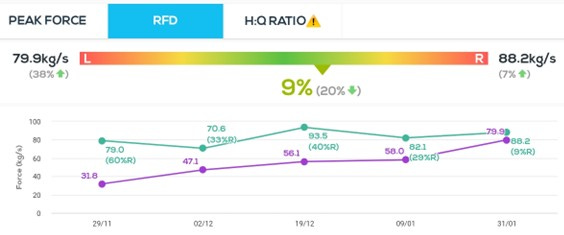
3. His Rate of Force Development (RFD) was returning fast.
We don’t normally see RFD come back before Peak Force in rehab.
To me, that was a sign that we might have found a long-term weakness of his hamstrings.
Without the Dynamometer, patient pushes hard against me as I hopefully try to hold him still– whilst conducting a Manual Muscle Test as I get flung across the room, I’ll call him a “4 or 5” say “job done” and off he goes until *twang* another hammy. S&C and Track Coach chooses another Physio to send their Athletes to.
But with the Dynamometer, this patient had had 50% limb symmetry. Not something we return patients to sport with. We pushed out timeframes for return to competition whilst we caught up this hypothesised long-term deficit.
Wally ran fast.
Wally lived happily ever after.
Let me tell you about Cindy the Centre, she runs and stops, a lot.
Cindy the Centre – Netball
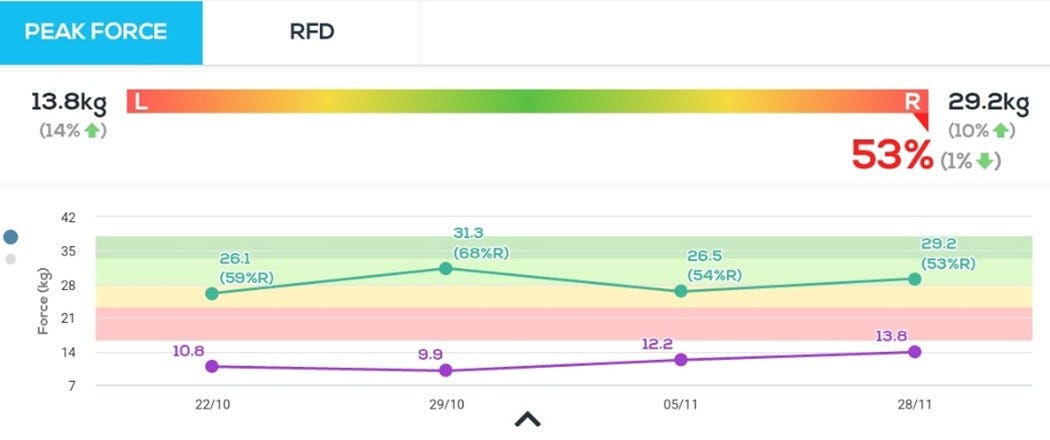
Cindy had a Kneecap Joint Whoopsie, which is a scientific term for an ‘instability episode of her patellofemoral joint, during a netball game.
She came in a week later reporting that her knee felt like it gave way at that time, and she felt a pop, it’s been a bit wobbly, now it hurts to go up and down things.
MRI demonstrated patellofemoral joint effusion, intact MPFL with a high signal, sub-chondral oedema behind the patella under a patch of “grade III chondromalacia” and an educated guess by the radiologist there was “a recent subluxation episode”
Oh boy, they’re smart cookies, those Radiological Wizards

We did Patellofemoral joint 101 stuff – Cindy felt better. She said, “I feel better can I play tonight.”
No. Nope. Nopey No No. Because Cindy did not look better.
On a step-up test she said “no ouchy” but she was stepping up with a hip dominant strategy (lots of hip flexion to use glutes to get up).
I said, “hmmm Cindy, it doesn’t look good... can you step up again with an upright trunk,” she said “no … it’s ouchy…. But can I play?”
We did an isometric knee extension test it was significantly weaker (55% off symmetry). She saw the live results on the tablet (they’re connected via Bluetooth to the dynamometer) she said, “I’ll do it again”.
She tried her darndest to push harder and managed to get the 4th purple dot below:
I said, “listen, we’ve got to get this good before you return – you might have already been carrying this weakness before you hurt it… I think the risk of you getting hurt again with a worse injury is high. It’ll take some time, but we’ll get there. “
And over 3 months, we did: (4th dot above = 2nd dot below)
She was happy.
I was happy.
Pharrell was happy.
Again, with no dynamometer in this situation, if I only ‘felt the force’ with my hands and said “you kind of feel weak” Cindy wouldn’t have believed me and would have left and:
1) Played with a significant knee extension force production deficit (aka “weak quads”)
or
2) Got a 2nd opinion from a Physio who’s a MMT Jedi down the road and had clearance to return to sports with a significant knee extension force production deficit (aka “weak quads”)
And then possibly ended up with a more significant knee instability injury.
Final Thought: Don't Be a Jedi, Be a Clinician
Dynamometry isn't about tech for tech’s sake—it's about making better clinical decisions, smarter rehab choices, and keeping athletes like Wally and Cindy on the field, not on the table.
Sure, there’s fancy gear that measures every breath your patient takes—often fitting the "all the gear, no idea" stereotype. But dynamometry isn’t about data overload; it’s about Clinical Pixels. Without these pixels, you’re left staring at a clinical picture that’s blurry, at best – missing, at worst.
A Dynamometer is one tool, but an important one, in a good Clinicians ever-developing toolbox. Data gained from Dynamometry provides many Clinical Pixels that form a Clinical Picture that is rarely complete, but without these Pixels, it makes it much harder to hypothesise what you’re looking at.
Sure…you can still use Manual Muscle Testing… just like you can still use a fax machine.
But if you’re still manually testing in 2025 to guide rehab decisions, and you work in Msk Physiotherapy and have a caseload of active patients, then ask yourself:
"Am I assessing, or am I guessing?"
And if your ego is still writing strength scores your dynamometer can’t cash—well… I don’t know what to tell you.
Unless, of course, you’re a Jedi.
You already know.
You knew the entire time.
You know?
Cue Star Wars theme, roll credits…
References
1. Norris R, Morrison S, Price A, Pulford S, Meira E, O'Neill S, et al. Inline dynamometry provides reliable measurements of quadriceps strength in healthy and ACL-reconstructed individuals and is a valid substitute for isometric electromechanical dynamometry following ACL reconstruction. The Knee. 2024;46:136-47.
2. Ashworth B, Hogben P, Singh N, Tulloch L, Cohen DD. The Athletic Shoulder (ASH) test: reliability of a novel upper body isometric strength test in elite rugby players. BMJ Open Sport & Exercise Medicine. 2018;4(1):e000365.
3. Bohannon RW. Reliability of manual muscle testing: A systematic review. Isokinetics and Exercise Science. 2018;26(4):245-52.
4. Hayes KW, Falconer J. Reliability of hand-held dynamometry and its relationship with manual muscle testing in patients with osteoarthritis in the knee. Journal of Orthopaedic & Sports Physical Therapy. 1992;16(3):145-9.
5. Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. British journal of sports medicine. 2014;48(22):1613-9.
Did this challenge your thinking or add value to your patient care? If so, even a small contribution helps me keep content like this going.
If this post helped you rethink an approach, refine a diagnosis, or improve patient outcomes, consider supporting my work.
☕ Buy Me a Coffee to say thanks, or become a paid subscriber—healthcare providers who subscribe can share cases with me or ask clinical questions anytime.
Tailor your Nick Ilic | Physio Clinician subscription:
You can customise which topics you receive updates for by selecting 'Manage Subscription' in your Substack options (in your browser), or by clicking 'unsubscribe' at the bottom of any email—don’t worry, it won’t unsubscribe you immediately! You'll then be able to choose your preferred sections:
✅ Patient Playbook
✅ Clinician’s Corner
✅ Research Reviews
✅ Clinician’s Compass
Choose what suits you best—I promise I won’t take it personally!