Clinicians Corner | Hipnosis - When Their Hip is Gaslighting You
Let It Go: The Hip Doesn’t Need More Stretching
Oh how I ‘ummed and ahhed’ about this one.
To Paywall or not to Paywall, that is the question—
To be tight, or just inflamed and misdiagnosed?
On one hand, hip joint pain is one of the most poorly managed conditions in MSK healthcare, and this kind of info is exactly the sort of thing I should be hiding behind a paywall. It’s valuable.
But on the other hand, hip joint pain is also one of the most poorly understood conditions in MSK healthcare—especially by the general public. The myth of “tight hips” continues to derail rehab, and patients end up stretching themselves deeper into dysfunction.
So here you go: no paywall. Just insights I believe are worth spreading—to clinicians, to patients, and to anyone who’s ever had a hip whisper “it’s the flexors” when it was clearly the joint.
💡 If you find this helpful, consider subscribing to my Substack for more in-depth clinical content, exclusive case studies, and professional insights.
Your support helps me continue sharing everything I’ve learned in the clinic with the world.
☕ Prefer a one-off thank you? Buy Me a Coffee.
Are you a patient with hip tightness, pain or discomfort - check out this patients guide:
Some joints are refreshingly honest.
The knee, for example, tends to be quite forthcoming—swells up when it’s irritated, gives way when it’s unstable, and generally makes its feelings known.

The hip? Not so much.
The hip is a deeply embedded joint, and it plays by its own rules. It refers pain in wild and inconsistent directions. It presents with vague “tightness” that leads patients (and sometimes clinicians) to stretch it into further dysfunction. And it’s often the last place we think to look—even when it’s been yelling the whole time.
This is hipnosis—where the hip sends distorted messages, gaslighting both the patient and the practitioner. And this is probably what makes it the most poorly managed Big Joint in the Msk Healthcare - especially in any therapeutic trade that likes to treat feelings and symptoms.
The Hip’s Greatest Tricks
A cranky hip joint doesn’t always say “hello” in the anterior groin. In fact, it often says hello somewhere else entirely:
The knee (especially medial - trust me, I know about that one)
The groin, anterior thigh, or saddle region
The deep buttock, even mimicking SIJ or lumbar referral
Occasionally, even down to the foot (just to mess with you)
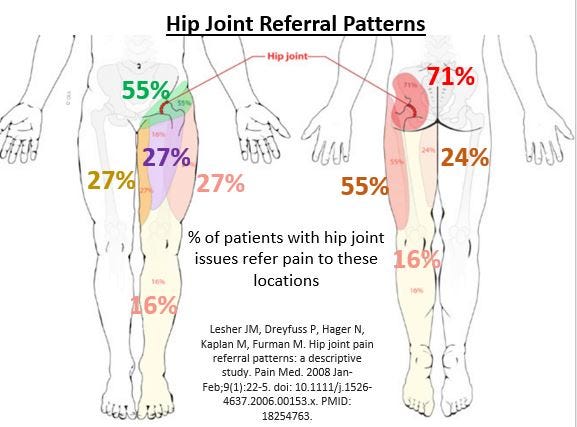
The spectrum of feelings ranges from tightness, achiness, and stiffness to vague heaviness or deep glute grabbing sensations.
One of the most underappreciated facts about the hip joint is this: it can feel “tight” when it’s actually inflamed (eg: Synovitis/Capsulitis).
And that tightness? It's not fixed by stretching it’s often made worse.
Gaslighting in Action
Patients with hip joint pain often say things like:
“I’ve been stretching my hip flexors daily, but it’s not helping.”
“I foam roll my glutes every night but it’s still tight.”
“It hurts in my knee… but the scan says my knee’s fine?”
“My yoga teacher says I’m tight, but I can do the splits.”
That’s the hip whispering misinformation through the walls of the joint capsule and soft tissue.
Hip joint pain doesn’t always localise.
It’s deep, muffled, and often distorted on its way to the surface—kind of like someone yelling underwater at a boat above.
You can hear something... but it’s hard to tell where it’s coming from or what exactly it’s trying to say.
How to Tell When the Hip Is the Culprit
To catch a cranky hip, you need to rule out the better storytellers first.

✅ Rule out the lumbar spine:
All good with flexion in standing/extension in standing/seated rotation?
No radicular signs?
SLR and slump clear?
Then it’s probably not the back.
✅ Rule out the SIJ:
No single-leg provocation?
Negative cluster (thigh thrust, distraction, compression, Gaenslen's)?
Move on.
✅ Rule out tendons:
No lateral hip pain with lying, stairs, and single-leg stance?
Gluteal tendinopathy cluster (GT palpation, SL Stance, FADER) positive?
Maybe. But if the pain is vague and refers widely, suspect the joint.
If you’d like more ideas on how to best differentiate the Lumbar Spine, SIJ and Hip Joints on assessment, I have a ‘Differential Diagnosis of the Hip, SIJ, and Lumbar Spine’ blog coming out soon - keep an eye on my Substack page.
Signs You’re Dealing With a Cranky Hip Joint
Pain with or after prolonged sitting or cross-legged positions
Feels better with walking or running
Worse with deep flexion, twisting, or long car trips
Anterior groin, thigh to medial knee, or deep glute symptoms
Loss of Adductor pain-free force production is common (>20% on dynamometry)
Positive FADIR Test (full flexion + adduction then slowly internally rotate…and watch their face for the eyeballs of doom)
(Caution: discomfort with FADIR is normal in active populations anyway, but how is it compared it the other side?)
And don’t forget:
"Hips can improve ROM simply by getting better."
Once inflammation settles, the capsule regains pliability. Don’t confuse restricted range with “tight muscles”—it’s often just joint irritability.
By the way, it’s worth mentioning - the FADIR test is very sensitive at ruling out intra-articular causes of hip pain
✅ Rule out hip joint:
Pain-free FADIR test, in the presence of full pain-free flexion + overpressure, and no pain with FABER (flexion, abduction and external rotation)…..
Rethink things. It’s much less likely the hip joint.
Management Tips – Stop Feeding the Fire
When the hip joint is inflamed, don’t stretch it.
(I know… EVERYONE does it… but just have a go at NOT doing it for your next few hip patients. Trust me - The Guy on The Internet You Probably Haven’t Met)
In fact, the first job is often convincing the patient to do less, not more.
🪑 Sitting Strategy
High-density foam wedge to reduce flexion
Limit prolonged sitting and cross-legged positions
Track sitting tolerance as a meaningful outcome measure
🧘 Interrupt the “Stretching = Fixing” Narrative
Glute tightness ≠ glute shortness
Psoas tension ≠ hip flexor tightness
Stretching into pain feeds the fire—itch-scratching behaviour feels helpful but delays recovery
“If stretching was the answer, they wouldn’t be in your clinic.”
🏋️ Load Smarter, Not Lighter
Modify depth, not resistance (e.g. squats to box)
Strengthen hip flexors, adductors, and abductors
Avoid heavy end-range positions in gym bros with FAI who insist on ass-to-grass

🎯 Avoid Over-Stimulation
Foam rollers, massage guns, spiky balls—it’s not always release; it can be re-aggravation and over-stimulation
I recently had one young tennis player’s 12-month buttock tightness++ (with constant thera-gunning, poking, rolling) simply resolve with two weeks of leaving it alone
⏳ Be Patient ..for the patient
Hips just take longer. They take longer to become symptomatic. They take longer to become asymptomatic. If you think 8 weeks for a knee, think 4 months for a hip. Set the bar low, set the appointments apart longer (patient will be fine… and in control of their hip-health week, they can email you if they need you) and chase those solid objective measures you noted in the first couple of appointments.
To Image or Not to Image?
In younger adults, hip MRIs are often unnecessary unless there’s been trauma or high suspicion of structural instability (e.g. labral tears, dysplasia).
Most cases of vanilla hip joint referred pain are diagnosed clinically with history, behaviour patterns, and a good assessment.
Trust me, once you’ve seen one Cam Lesion type patient, you’ll know who they are. In supine, you’ll slowly take their knee up to their chest and it will start winging out into abduction from 80-90deg. It just won’t track in a straight line along textbook flexion.
Red flags still apply, especially in the ‘Paeds-Pop’ (Slipped Capital Femoral Epiphysis, Perthes, etc.)—but for the average adult presenting with vague hip/groin/knee/buttock tightness and no clear mechanism, start by calming the joint and listening to what the joint says.
And please, ensure you take a good history clear any Developmental Dysplasia of the Hip (DDH), especially in those loosey goosey patients - you know the ones, they always complain they’re “tight” but can pull their leg over their head.
Young Males, think FAI spectrum. Young loosey goosey Females, think DDH spectrum.

Eg: A Loosey Goosey with a “Tight Ass”? If there’s no posterior acetabular coverage that ball just keeps pissing off the back of that socket (posterior capsule).
Case in Point: Treat the Patient, Not the Scan
A few years ago, a 35-year-old gentleman came to see me for a second opinion on persistent hip pain. He was 12 months post-op following arthroscopic removal of a cam lesion for Femoroacetabular Impingement (FAI).
His original physio had spent the better part of a year trying to stretch and release the “tightness” away. Glute strength? They hammered it. Repeatedly. When symptoms didn’t budge, he was labelled as having “failed rehab”. An MRI was ordered and a ‘cam lesion was found’ and a surgeon was only too happy to shave off the bony prominence found on imaging.
Back to physio he went. Same approach. Cam lesion gone now, so surely it would work this time… right?
Spoiler: Same pain.
By the time he saw me, three years had passed since onset. Not one provider had recommended:
Sitting less and standing more
Avoiding deep hip flexion under load
Ceasing aggressive stretching and soft tissue work
Backing off the Theragun/massage gun blitz
With a short course of oral NSAIDs via his GP and a basic strategy of activity modification, load control, and hip position awareness, his symptoms resolved in four weeks.
Moral of the Story:
Sometimes the simple stuff works best.
”Failed rehab” is can sometimes be failed reasoning.
And when you treat the scan, not the patient—you may miss the point entirely.
Hip Exercises?
Yep…I know them. I know some of you are desperate for the one or two that fixes all the things - but it’s outside the scope of this particular blog.
I do have a process for targeting hip (and more global) deficits with rehab based on dynamometry testing and biomechanical analysis (of whatever athletic action they’re doing).
The point of this blog was: See how far ‘Good Management’ can take you with these patients - the useful thing is: most of them have already done all the other stuff anyway so are happy to go with Advice/Education and Activity Modification (+/- oral NSAIDs).
Go get into some of the fine work (and the paid coursework) of these Hip Experts: Alison Grimaldi, Mehmet Gem aka The Hip Physio, Enda King, Andrew Wallis and the team at The Hip & Groin Clinic…. just for starters - there's many others who started opening my eyes up to this stuff years ago.
Final Thoughts: The Joint Whisperer’s Challenge
The hip joint doesn’t shout. It murmurs, misdirects, and refers.
It mimics other structures, hijacks other referral patterns, and leads patients (and clinicians) down unhelpful rabbit holes—unless you’re tuned in.
So if the tests are vague, and the story doesn’t fit, and the patient swears it’s their tight hip flexors but stretching only gives short term relief but long term ‘itch’…
…it might just be a hip joint gaslighting everyone involved.
If this piece made you stop stretching a hip this week, I’ll consider it a win. If it made you rethink your whole approach to hip pain—welcome to the club.
Got a tricky case you’re stuck on? Drop a comment, share your thoughts, or hit reply.
This was an update on:
Did this challenge your thinking or add value to your patient care? If so, even a small contribution helps me keep content like this going.
If this post helped you rethink an approach, refine a diagnosis, or improve patient outcomes, consider supporting my work.
☕ Buy Me a Coffee to say thanks, or become a paid subscriber—healthcare providers who subscribe can share cases with me or ask clinical questions anytime.
Tailor your Nick Ilic | Physio Clinician subscription:
You can customise which topics you receive updates for by selecting 'Manage Subscription' in your Substack options (in your browser), or by clicking 'unsubscribe' at the bottom of any email—don’t worry, it won’t unsubscribe you immediately! You'll then be able to choose your preferred sections:
✅ Patient Playbook
✅ Clinician’s Corner
✅ Research Reviews
✅ Clinician’s Compass
Choose what suits you best—I promise I won’t take it personally!