Clinicians Corner | Let’s talk about a Radicul-ous condition called ‘Armatica’
What’s the difference between Radicular Pain, Radiculopathy, and Spinal Referred Somatic Pain, and why does it matter?
This post would typically be behind a paywall, as it contains highly valuable, evidence-based insights and clinical recommendations. However, I believe this condition is often mismanaged, and better awareness is needed—so I’m making it freely available.
If you find this post valuable, subscribe to my Substack for more in-depth clinical insights, exclusive case studies, and expert guidance. Your support helps me continue sharing practical, experience-backed knowledge.
☕ Prefer a one-off thank you? Buy Me a Coffee.
This post is a guide only and should not be taken as medical advice. It does not replace assessment and recommendations from a registered and regulated healthcare professional.
5 years ago, roughly halfway through my 2nd career/hobby as a Musculoskeletal Clinician and Physiotherapist, I refused to see any more neck and upper limb neural pain patients.
I had over-treatment fatigue and felt I was ill equipped by tertiary education and ongoing education (what was available at the time) to manage neck and upper limb nerve pain patients well.
At the time, I was also having pain in my right (dominant) thumb, so I used that injury as an excuse to stop seeing patients, to “give it a break” from all those cervical spine mobilisations and localised soft tissue work/massage.
But really, I just wanted time away from neck patients. Little did I know, having a one-year off-season from seeing neck patients would be one of the best moves of my career.
What was also useful at that time was my first-hand experience with neck pain and referral into my shoulder. Which I swear was my shoulder, even as someone who knows what’s really going on.
During that Neck Off-Season I came across the material in this blog which has significantly helped me get better outcomes for my patients with Spinal Referred Pain and Nerve Root Referred pain. It has allowed me to mature even further as a healthcare professional (despite the increasing immaturity as I age — blame my young kids for that). As a result, I have a greater appreciation for my role in healthcare and am even more satisfied with my career.
I hope this article helps someone out there the same way it helped me, even if it’s a patient searching for answers.
Disclaimer
This blog is very much The Broad Strokes. This is an extremely complex topic and I’ve only licked off the Icing on the Complexity Cake. However, that does nothing to take away from the fact that the contents in this blogpost are not well recognised or known. By presenting the basics it could potentially have a big impact on the lives of patients with Spinal Referred pain without going into much depth.
Not only is there ‘broad strokes’, I have also intentionally reduced the human pain experience down to biological causes, and modern pain science teaches that there are many biological, psychological and social contributors to the pain experience (aka BioPsychoSocial).
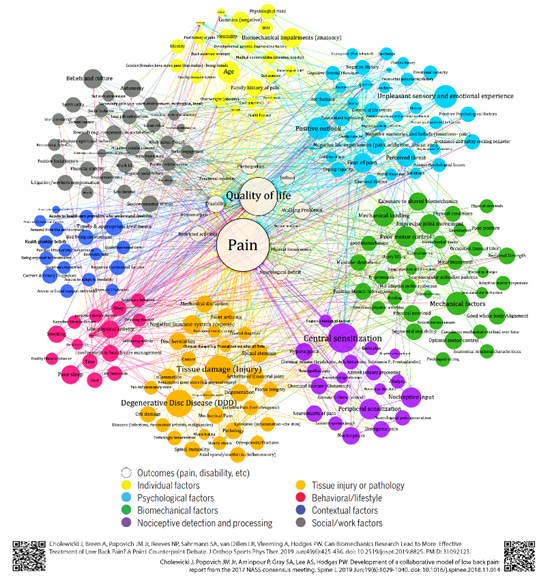
So, I will now clearly admit that this blog has a Bio focus and for good reasons, outlined below.
Introduction
If there was a formula which was:
and we generated a list of common conditions causing pain and dysfunction, then Spinal Referred Pain, Spinal Radicular Pain and Spinal Radiculopathy would be somewhere on top of the list.
The fact that these terms and diagnoses, and their management pathways, are not well known is totally Radicul-ous (…see what I did there?).
Spinal Referred Pain
Spinal Radicular Pain
Spinal Radiculopathy
What is downright bizarre and crazy was that I didn’t understand what most of these terms were until years into my career…. or how they helped in the management of what is often a complex musculoskeletal +/- neurological pain condition, and it’s not from a lack of education. I must spend 100s of hours on my CPD each year, reading articles, going to conferences, listening to speakers and podcasts. We certainly didn’t cover these conditions at university.
Let’s Get to the Root of the Terminology
Those of you who do know about Radicul-ous stuff will know the joke in that heading ( …root).
Radicula = ‘Little Root’ in ye olde language. Related to Radical in middle English.
So lets get a bit radical and root around with the word and see what happens:
Radicular Pain — Pain from the Root
Radiculopathy — Problem with the Root
Referred Pain — A couple of words used in the musculoskeletal and medical world to indicate a pain, experienced by the patient in one region, that is likely stemming from another region (eg: ice cream headache). Eg: Rotator Cuff Referred Pain, Kidney Referred Pain, Lumbar Spine Referred Pain, Patellofemoral Referred Pain.
Types of Pain
Somatic Pain
Cervical Referred Somatic Pain is the correct term for what I call “vanilla neck pain” (or vanilla back pain for Lumbar Referred Somatic Pain).
You’ve probably heard the word ‘somatic’ lumped in with Psychosomatic in the past; somatic means ‘from the body’ instead of from the mind. You may also see it interchangeably used with ‘nociceptive pain’; nociception simply refers to the radars of our body, our early warning system. Nociceptive nerve fibres send warning messages to our brain, which are interpreted as either false alarms, or as danger, which generates ‘Pain’ as an output. (This pain theory is currently under debate again, but for the sake of moving on with the blog, let’s carry on).
Somatic pain is pain experienced in the local region, not always focally (<5cm area) or very locally (eg: low back pain is rarely right over the spinous process of L5) . Both neck pain and low back pain are much more likely to spread out into the surrounding area. The upper traps for the neck, or the buttocks and love handles (or quadratus lumborum muscles, latin for ‘love handles’) (….ok it’s not really, but amor manubrio is).
Somatic pain is usually low on the irritability scale, perhaps 1–5/10
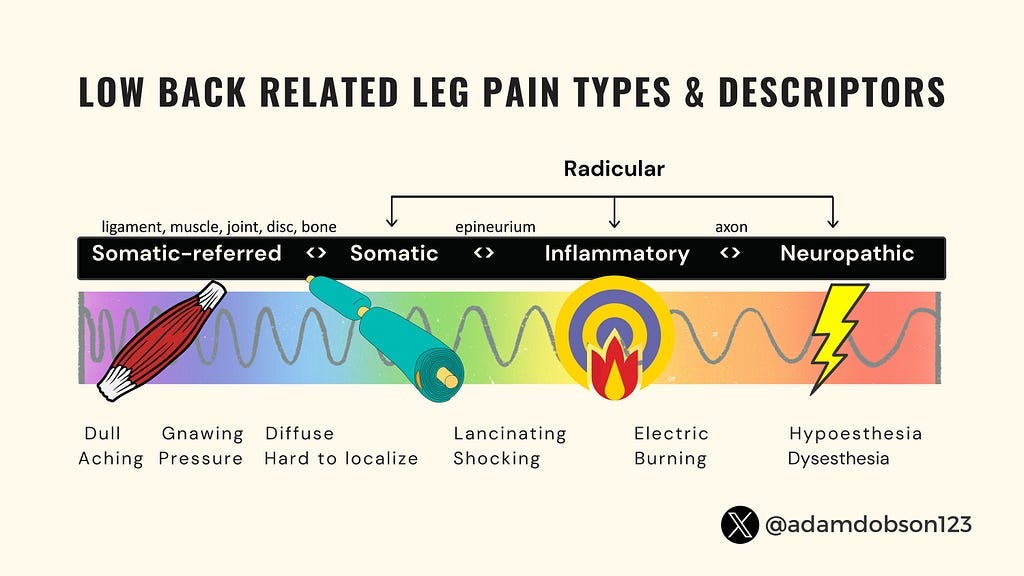
Somatic pain can come from a variety of issues with the tissues (aka ‘triple ply’) or even just a single tissue (aka ‘single ply’).
Neuropathic Pain
It doesn’t take an Einstein to work out that pathic probably means something nasty, and neuro means nerve, and if you ask anyone with Neuropathic Pain they’ll tell ya: “It’s nasty nerve pain”.
Neuropathic pain is usually more intense (>5/10 up to the infamous “11/10”… some people just love to give 110%). Neuropathic pain tends to radiate out along pathways following the nerve downstream from where the problem is (otherwise known as “shit rolls down hill” — a handy term to consider when diagnosing other conditions such as Carpal Tunnel Syndrome (wrist to thumb/finger) or Cubital Tunnel Syndrome (elbow to little finger)).
Where exactly are we talking about?
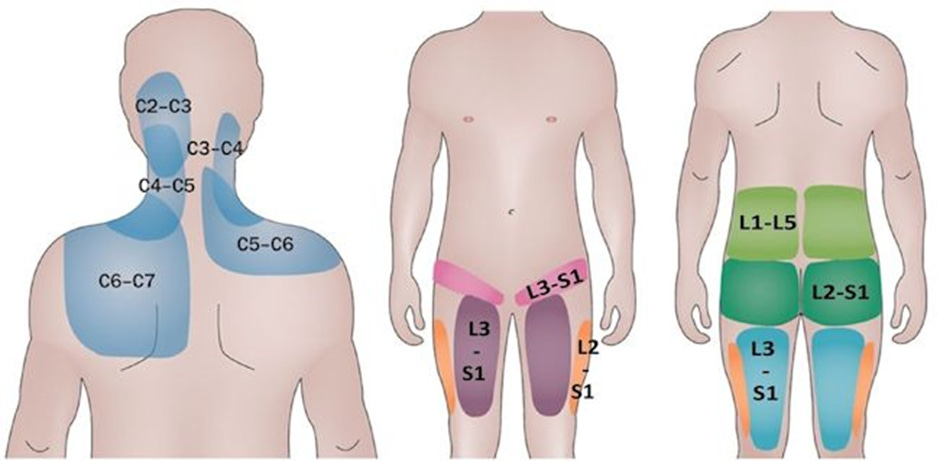
When talking about Spinal Radicular neuropathic pain it is related to the Spinal Nerve Root(s) — extensions of the spinal cord that branch off through little windows (called foramen) in the spine. We have 31 pairs of them, represented by the blue branches leaving the spine on the below picture.
When they decided to name them they must’ve let the work experience kid do it that day, because in the Cervical spine the nerve root is named after the segment BELOW it (C1 nerve root is above C1 vertebral body), except C8 nerve root which is under C7 (there is not C8 vertebral body). And then the nerve roots are named for the segment ABOVE them, example L5 nerve root is below the L5 vertebral body (and above S1).
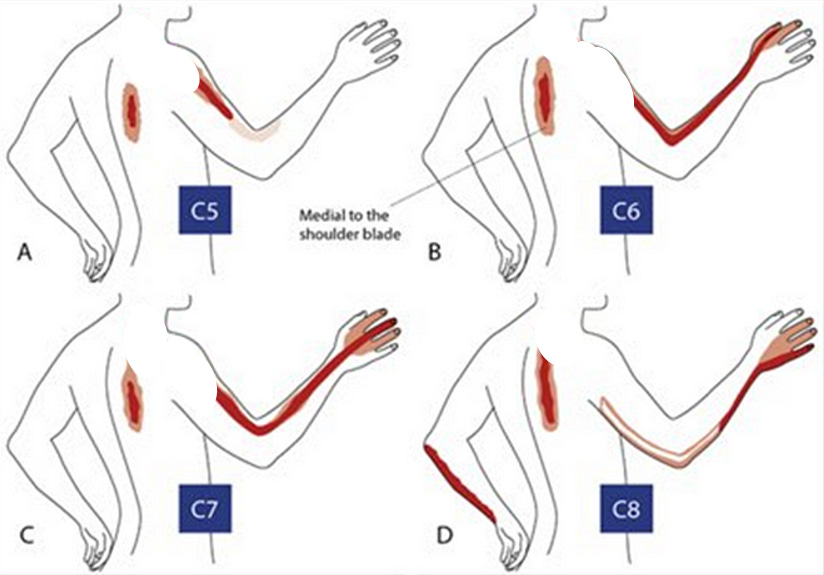
Common Radicul-ous sites causing referred pain into upper and lower limbs are: C6 and C7 in the neck and L5 and S1 in the lower back.
Let’s jump back to the Radicul-ous stuff (btw, if you see “radicul-ous” in use after Feb ‘24, you saw it here first).
Let’s Get Radicul-ous
If you’re like me (and for God sake I hope you’re not, for many reasons, greying hair and balding for starters) you’re probably wanting to get super comfortable with:
The Difference between Radicular Pain and Radiculopathy
so here we go:
Radicular pain
Radicular Pain is neuropathic pain arising from an irritant and inflammation of the spinal neve root. Technically it is an abnormal ‘gain’ in function of the nerve which includes pain, but can also include paraesthesia, hyperalgesia, allodynia, hyperreflexia, and/or muscle spasms. It may or may not be from a mechanical cause such as compression primarily. This painful condition usually has a prognosis or natural history that is longer than Spinal Referred Pain. However, there may not be any injury as such, it is often just a ‘sensitisation’.
For those of us who were dating in the 90s/00’s, you’ll know the derogative term SNAG — a sensitive new age guy. Well Radicular Pain isalso a SNAG, it’s a Sensitive Nerve And Ganglion. (oh dear, THAT was a very niche neurology joke)
The other interesting thing about radicular pain is that it’s highly likely to not cause pain near the spinal nerve root, where the spinal referred pain region is. Cervical Radicular pain is mostly likely to occur down the arm, usually past the lateral elbow into the forearm — mimicking and often confused as tennis elbow, or given the vague and non-helpful term of ‘RSI’ . It can also appear in the shoulder blade, well away from the neck.
We see this with Lumbar Radicular Pain, it starts at the gluteal fold (the bottom of your bum) and travels down, and it does not appear in the lower back.
Liaison with a good GP is often required for amedications review, including oral anti-inflammatories (NSAIDs). An MRI may or may not be appropriate, however if the condition progresses or worsens an MRI will usually be ordered and if oral NSAIDs haven’t taken the edge off, a CT Guided Cortisone injection at the nerve root might be also considered months later.
Radiculopathy
Radiculopathy is a motor or sensory dysfunction related to a spinal nerve root which is not painful, and can be from a mechanical cause such as compression from a disc or the foramen (the window/tunnel it travels through) or another space occupying lesion (something else in there, that shouldn’t be there, taking up space).
An example of a motor dysfunction would be gross weakness such as a lack of knee extension strength (patient trips over a lot). It won’t be completely absent though as we have some redundancy built in since both L3 (mostly) and L4 (some) contribute to motor (motor = movement) function of the quadriceps.
An example of a sensory dysfunction would be loss of feeling to touch, or even tingling in limbs in the distribution of the nerve root.
Radiculopathies require urgent medical investigation as they usually indicate more significant and injurious conditions with a much longer prognosis or natural history than both Spinal Referred Pain and Radicular Pain.
This usually requires an MRI at least, nerve conduction studies and a Neurospecialist Consult with the possibility of surgery such as discectomy or decompression.
It’s apples and oranges, but sometimes it’s a fruit basket
So radicular pain is painful and radiculopathy is not.
Spinal Referred Somatic Pain is local, and Radicular pain and Radiculopathy are not.
Radiculopathy can present with weakness and/or sensory changes, and radicular pain and spinal referred pain do not. (I’m temporarily and conveniently disregarding pain inhibition weakness for now to help keep things clear).
Spinal Referred Somatic pain arising from cranky non-neural tissues, has a good prognosis (usually short-term, < 3months) and doesn’t normally warrant further investigations or prescribed medications.
Spinal Radicular pain arises from sensitised and usually inflamed spinal nerve roots and has a medium to long prognosis (6months-2 years) and is usually assisted with prescribed medications (oral NSAIDs).
Whereas Radiculopathy arises usually from ongoing compression and injury to a spinal nerve root and usually has a longer prognosis (1year+) and may require further investigations and sometimes surgery.
Therefore ‘it’s apples and oranges’ right? Nope!
Thanks to the complexity of the human body and its owners, often it’s not apples and oranges, it’s a fruit basket.
These conditions can and do often co-exist. It’s helpful clinically when someone trips into the clinic with a ‘Vanilla’ Radiculopathy (e.g.; left L5 radiculopathy causing weak dorsi flexors — the muscles that lift your foot up so you don’t trip over, +/- numbness down the outside of the foot).
But often they’ll have Spinal Somatic Referred Pain as well as Radicular Pain. Or just radicular pain as well as Radiculopathy — which brings us to a very infamous pseudo-medical word which has wide usage (for good and bad) by both the public and the medical community:
Sciatica
“Hang on! Isn’t all of that stuff you just mentioned similar to Sciatica?”
Sciatic is an umbrella term used by the medical community and therefore has been adopted by the non-medical community en masse.
Like all umbrella terms they are a double edged sword: They point in the right direction but usually don’t help you down the right path.
Sciatica is used to interchangeably describe BOTH radicular pain and radiculopathy. But I also think some less learned members of the medical community also clump Spinal Somatic Referred Pain under “Sciatica” as well.
But it’s not all doom and gloom, I’d prefer there be a well known term like Sciatica for what is essentially: (Best read in a Dumbledore voice) A term which describes pain from a neural issue arising from somewhere in the sciatic nerve, which I think, if my memory serves me right, attaches to the lumbar spine in a few places.
What a common term does, because it’s well known, it’ll either be used as a True Positive (e.g.: A patient given the term Sciatica as a diagnosis for their posterior lower limb neural pain arising from their spinal nerve root) or a False Positive (e.g.: a patient given the term Sciatica as a diagnosis for their posterior lower limb pain which arises from the proximal hamstring tendinopathy which was missed).
What I’m getting at is: It will not be missed (but sometimes will be mis-attributed).
Which is good I think, because as Oscar Wilde once said:
And do you know what is NOT being talked about, therefore is often missed:
Upper Limb Neural Pain arising from the Cervical Spinal Nerve Root(s) — aka:
Cervical Spine Radicular Pain
so….
Exclusive Premiere of a New Medical Term: Armatica
You read it here first.
Armatica, it’s Sciatica for the arms.
My brainstorming also included: HighAtica (high sciatica), Brachiala or Brachial Plexica (sciatic nerve gets sciatica, brachial plexus deserves some love too).
“What point are you trying to make here?”
Oh right, thanks.
If we had a name for it (Cervical Spine Radicular Pain) maybe it would be not missed so much. I’d even be happy for some mis-attribution. I’d be happy if a bunch of patients came in for 2nd opinion of their Armatica and it turned out it was Lateral Elbow Tendinopathy (tennis elbow) all along! That’d honestly make me cry tears of joy, which would be a nice change from my tears of woe from all these years of seeing:
Tennis Elbow patients who had Cervical Spine Radicular Pain*
“RSI” patients who had Cervical Spine Radicular Pain*
Golfers Elbow who had Cervical Spine Radicular Pain*
Capral Tunnel patients who had Cervical Spine Radicular Pain*
*also now known as: Armatica
The reverse has been happening for years. As someone who until recently was The Tennis Physio (dot com) I was getting referrals from across town and the surrounding region for ‘Tennis Elbows’ (lateral elbow tendinopathy) that weren’t getting better.
At least 75% had Armatica (Cervical Spine Radicular Pain).
Golden Clinical Rule: “If it’s both sides, look in.”
There’s a great rule in musculoskeletal diagnostics:
If a patient reports pain going into both limbs, look in.
If they have “shoulder” pain on both sides, check the cervical spine.
If they have buttock or posterior leg pain on both sides, check the lumbar spine (and rule out CES).
What boggles my mind is I’ve seen patients with “left and right side golfers elbow” and they’ve been seen by multiple practitioners and no one has checked the neck over years. Not a single one. One of these patients was about to get exploratory elbow surgery.
The Schneck
There is also a common presentation of what is called “Schneck Pain”, which is when the patient reports “shoulder” pain, however they indicate a distribution of pain which the shoulder (glenohumeral joint) doesn’t refer to, and is instead Cervical Spine Somatic Referred Pain that has been misdiagnosed.
Clinicians Corner | When is a Shoulder not a Shoulder
Why labels matter in the differential diagnosis of Neck and Shoulder pain.
I have seen this lead to some quite serious malpractice (e.g.: shoulder surgery for neck pain) leading to long-term disability, pain and dysfunction for the patient. Simply because multiple practitioners did not clear the Cervical Spine for the “shoulder” pain.
What’s even crazier, some of these missed diagnoses didn’t just have Cervical Spine Referred Pain referring near the shoulder, but they also had radicular pain down the arm into the hand….. which the actual shoulder (glenohumeral joint) is highly unlikely to do.
This is covered extensively in my blog above, so I won’t rehash it here.
In an age where ‘Non-Specific (Region) Pain’ labels are on the rise, and “You don’t need a Diagnosis when it’s just symptom modification”, one must ask:
“Does any of this matter? Does a Diagnosis really matter?”
I’ve previously written on the specific vs non-specific aspect of diagnoses and injury management. I think we need to rule out specific conditions (especially Red Flag conditions) that have specific management pathways, and then we’re often left with non-specific management of pain arising from regions where management doesn’t change if we dig deeper to nail down what the exact issue is with what tissue. Speaking of ‘nailing down’….
The Law of Instruments (if all you have is a hammer, everything looks like a nail) has a negative effect in the medical and musculoskeletal world.
Part of the problem is that many practitioners out there don’t have good understanding across a breadth of conditions that cause pain and/or dysfunction.
To some practitioners, if it looks like a duck and sort of quacks like a duck, but it walks weird but maybe some ducks do that…. Then it must be a duck. But those practitioners have never seen or heard of a Swan, Goose, or a Waterhen — so suddenly everything is a duck.
(They certainly haven’t ever seen a Bogduk, or a 2009 Bogduk article called ‘On the definitions and physiology of back pain, referred pain, and radicular pain’).
(If you’re thinking, “wow Nick, you really went to great lengths there to slip in a terrible Bogduk joke then you’d be right).
Diagnosis matters and umbrella terms can be a pain, literally.
If Doctors don’t know what Cervical Spine Radicular Pain (aka Armatica — yep….I’m persistent) is then they’ll just call that vague arm pain near the elbow: Tennis Elbow, send it to physiotherapy where some well meaning new graduate will make the patients do stretches (which sensitised nerves don’t like) and grab a dumbbell and go up and down and up and down. Until 4 years later they finally run into a healthcare practitioner who knows about Radicul-ous stuff and finally gets them on the right management pathway.
What recommendations I give to rehab providers
Somatic Referred Pain
Rehab providers are usually pretty experienced with dealing with Vanilla Neck or Back pain, which is usually Spinal Referred Somatic Pain. They stay away from aggravating positions and provide exercises that gradually restore those positions and generally keep them moving. This is where the term Non-Specific Low Back Pain enters the arena. It’s a term that is (hopefully) not provided to patients but used amongst musculoskeletal colleagues to describe low back pain where management doesn’t need to be specific based on whatever structure is causing the pain. This is convenient because usually we don’t really know what structure is causing the pain, it’s easy to go down deep and dark rabbit holes looking at “changes” on MRI when there are so many age-related changes on imaging in pain-free people based on a whole bunch of studies.
However I generally find for necks there’s a pattern where they do not like doing overhead push activities, where the elbow goes past shoulder height (such as shoulder press), and in early stages any particularly heavy upper limb tasks also stirs it up.
Radicular Pain
We’ve spent years throwing neurodynamic “stretching” otherwise know as neural sliders and gliders at these cranky nerves. The original idea was that the nerves were “stuck” and because we had a mantra “motion is lotion” we thought we could “unstick” them by getting the patient to do specific movements along the specific nerves pathway. Since then we’ve come to realise it’s not that simple and we probably don’t have to be that specific (uh oh… here comes “non-specific” again). There’s also a possibility that cranky nerves are not a fan of traction or being pulled. In fact in my clinical experience, they’re not a fan at all.
So I recommend we modify the daily activities and exercises where patients might traction the sensitised nerve (e.g.: sciatic nerve radicular pain will be annoyed with full Romanian deadlift, so we do mini RDLs instead).
Radiculopathy
Considering these patients might have something serious going on, such as something mechanical pressing on the nerve root, one might have to be extra careful in the exercise space with these patients. Once anything big has been ruled out then it’d be pretty similar to dealing with patients with Radicular Pain. The only caveats being caution in those whose sensory changes might cause a safety issue in a gym environment, or those with significant motor dysfunction or weakness will need to also be careful. However, I’d generally target that weakness (e.g.: knee extension with quads focused exercises) to try and get whatever neuromuscular activation we can in the absence of usually one spinal nerve roots input.
“Could you summarise this for me in a table please?”
Only because you asked so nicely:
“You didn’t mention the Thoracic Spine”
There doesn’t seem to be the same prevalence and long-term and/or significant presentation of Somatic Referred Pain, Radicular Pain and Radiculopathy from the Thoracic Spine.
A word of warning about this region: Tread Carefully. This is an area where infections like to hangout, and obviously there’s a bunch of stuff hanging out inside the thoracic cage which may present as musculoskeletal pain. However, these conditions be non-mechanical and once you probe further into their medical history you might get a few clues that something else is going on.
Summary
All regulated and registered healthcare practitioners who work with patients who experience pain or dysfunction should be aware of the terminology:
Spinal Referred Somatic Pain
Spinal Radicular Pain
Spinal Radiculopathy
In particular, the presentation (pain vs no pain, motor/sensory dysfunction or not), the prognosis (short, med, long-term, to set expectations) and management pathways involved with each (activity modification and exercise -> medications -> diagnostic imaging -> CT guided interventions -> nerve conduction studies -> surgical referral).
To reduce misdiagnosis and mismanagement of patients who are possibly going through one of the experiences of their lives:
Let’s save the umbrella terms for a rainy day.
Most importantly, the term ‘Armatica’ should forthwith be utilised at every opportunity, starting at grassroots with education sessions with kindergarten aged children and working our way up to childish healthcare professionals (and I self-identify as one).
Finally, I submit forth, new and novel terminology, the use of which will revolutionise musculoskeletal medicine and possibly even cure all diseases:
1. Armatica — Neural pain affecting the upper limb, caused by inflammation at the cervical spine nerve root(s). Sciatica but in the upper limb.
2. Radicul-ous — Referencing anything to do with radicular structures, particularly with a sceptical attitude.
3. Amor Manubrio (Latin, love handles) –to replace Quadratus Lumborum which is frankly Lum-boring.
Thanks, and Credit
Nikolai Bogduk https://pubmed.ncbi.nlm.nih.gov/19762151/
Tom Jesson https://tomjesson.com/
His books are HIGHLY recommended for a much better and deeper dive into this topic and more:
Honourable Mentions and Good Listens
The Words Matter Podcast — What’s in a name? Making sense of ‘sciatica’ with Tom Jesson https://pca.st/lgqfo234
The E3Rehab Podcast Ep 135. Questioning Neural Mobilization w/ Aaron Kubal — https://pca.st/6s69pwpl, and Ep 39. Disc Herniations & Sciatica w/ Tom Jesson — https://pca.st/g6uixys2.
Did this challenge your thinking or add value to your patient care? If so, even a small contribution helps me keep content like this going.
If this post helped you rethink an approach, refine a diagnosis, or improve patient outcomes, consider supporting my work.
☕ Buy Me a Coffee to say thanks, or become a paid subscriber—healthcare providers who subscribe can share cases with me or ask clinical questions anytime.