Clinicians Corner | Managing “Tennis Elbow” in the Middle Ages (2024-25 Update)
A 2024 update on management of Persistent Lateral Elbow Pain
*Lateral Elbow Tendinopathy aka Lateral Epicondylalgia aka Lateral Epicondylitis
This is a no-paywall blog post with insights I believe are valuable. If you find it useful, subscribe to my Substack for more in-depth content, exclusive case studies, and clinical insights.
Your support helps me continue sharing everything I’ve learned in the clinic with the world.
☕ Prefer a one-off thank you? Buy Me a Coffee.
This post is a guide only and should not be taken as medical advice. It does not replace assessment and recommendations from a registered and regulated healthcare professional.
This is an update on my thoughts and experience on managing patients with Lateral Elbow Tendinopathy, otherwise known as Tennis Elbow. Although the correct nomenclature for this condition is ‘Lateral Elbow Tendinopathy’ for the purposes of brevity and dissemination I will use the colloquial term ‘Tennis Elbow’ …. even though it irks me (as a nerd) deeply.
In August 2020 I wrote a comprehensive blogpost on Tennis Elbow as I had changed how I was managing patients with this condition, having been dissatisfied with the ‘usual care’ and library of exercises and treatment techniques which Physiotherapists were doing at the time (which some are still doing). Back then , I was working in elite Tennis, and also seeing a bunch of local recreational and advanced club players as “The Tennis Physio(dot com)”. Calling yourself The Tennis Physio of course means, to my healthcare network and the public in general, I’m considered an instant ‘Tennis Elbow’ expert on a painful condition which affects a whole bunch of people …..many of who never actually play tennis.
10 years ago we had a menu of different exercises to throw at patients. Stretches, eccentrics, the classic dumbbell wrist drop-off-the-table routine — it was after all the golden era of eccentric loading. The belief (taken out of hand from a handful of studies) was that eccentrics could fix all tendinopathies. Or perhaps Isometrics, because “nah eccentrics are rubbish, it’s now all about isometrics — 3x40secs holds!”.
Turns out, not so much. It’s a bit more complex than that.
Over the past 10 years, it appears not all tendons magically respond to eccentric and isometric resistance training the way we thought they did, nor can we expect to treat a tendon complex such as the common wrist extensor origin group like an Achilles Tendon in the heel or a Patella Tendon in the knee. Eccentrics and isometrics have their place; they are one tool in a giant toolbox for the management of painful soft-tissue conditions.
The Evolution of Tendon Thinking
Fast-forward a decade, and we’ve come a long way in our thinking yet seemingly nowhere in our management. We now recognise that lateral elbow tendinopathy behaves similarly to rotator cuff tendinopathy, gluteal tendinopathy, and plantar fasciopathy (aka Plantar Fasciitis) in the middle aged cohort (soon to be defined below).
The common thread? These conditions often appear out of nowhere, sometimes not even with a clear mechanism of injury such as “doing too much too soon”. These conditions particularly in the ‘Middle Ages’ — the 45–65 age group — a demographic that’s busy, time-poor, and often not exercising regularly.
For these folks, tennis elbow isn’t just about ‘overuse.’ It can pop up spontaneously, likely influenced by systemic factors like diabetes, poor sleep, inflammatory diets, and general tendon health. There’s a saying: the tendon is a barometer of the system — a phrase that makes you reconsider whether this is purely a local elbow issue.
*Insidious onset = came on slowly over time, unrelated to an immediate injury, may or may not be related to a “too much/too soon” mechanical overload.
The Mid-Life (Tendon) Crisis aka Tennis Elbow in the Middle Ages
This middle aged patient cohort are a very busy cohort of patients, usually in the peak of their careers, very time poor, usually busy with kids or grandkids and don’t have much time to spend on themselves. Often, but not always, they are not regular exercisers or gym goers, yet they develop a condition like Tennis Elbow, seemingly out of nowhere, where they have pain with gripping things in life.
Which can be pretty disabling in day to day life. Especially when you consider how many times you grab something with your dominant hand such a kettle, a door handle, a steering wheel, even more so if they are active gym goers and they have great difficult gripping gym weights for resistance training. Or, if they are in the very small cohort that do play tennis, particularly those with single hand backhands (most middle aged club players), they have pain on ball contact.
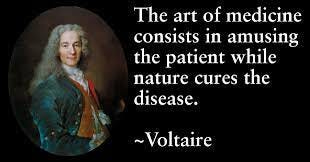
The Hard Truth: Time is the Real Healer
One of the biggest shifts in our understanding is that lateral elbow tendinopathy has a natural course to run. No matter what we do, it might take over a year (sometimes two or three) to resolve. Sometimes it can be weeks, usually this is where there is a clear “too much too soon” cause such as ‘pruning the hedges for hours on the weekend’. But more often, especially for the middle-ages cohort, it can be months or even over a year.
This is a tough sell in a world where patients want instant fixes and providers want to sell solutions to desperate patients.
So, what does work? Well, we know a few things:
Cortisone Injections — Great for short-term pain relief, but in the medium to long term, they often lead to worse outcomes. Repeat injections of Cortisones aren’t a good idea, cortisones are toxic to tendons (and cartilage in joints).

2. Hands-on/Manual Therapy — Also useful for short-term relief to allow patients to be more functional and do rehabilitation, but long-term, patients might end up in a similar same place with pain and function.
3. Strength? — Strong people get tennis elbow too. Strength doesn’t necessarily prevent it or predict who recovers faster (a hard pill to swallow for many rehab pros). However, there are many systemic benefits to resistance training (and exercise in general) that might impact tendon health long-term.
What’s Left?
Patients come to us for pain relief, and there are things that can help — just not in the way people might expect. Pain relief strategies should be individualised, starting with what has worked well for the patient in the past.
If massage helps, great.
If stretching works, fine.
If strength training does the trick, let’s do it.
The key is to empower the patient, not create dependency on hands-on treatment or gimmicky (and often expensive) devices.
Active strategies — things patients can do themselves — should always be prioritised over passive treatments like ultrasound, laser, or endless physio ‘magic tricks.’ The goal is to coach patients toward self-management, not keep them coming back for feel-good fluff.
The Problem With the “Fix” Mentality
A huge issue in treating tennis elbow is the false promise of a quick cure. Too many providers push miracle fixes that supposedly ‘heal’ tendons.
The reality? The condition takes time, and most treatments merely help manage symptoms along the way. Misleading narratives like “your tissues are tight and need loosening” do more harm than good, fostering reliance on ineffective treatments rather than giving patients real control over their recovery.
Anyone that says they can ‘cure’ or ‘fix’ your Tennis Elbow without having met you, are likely to be a charlatan.
The Systemic Connection
Why does this 45–65 age group seem to be ground zero for tendinopathies? Well, it’s the same demographic where systemic health issues — heart problems, diabetes, kidney disease, thyroid dysfunction — start creeping in, including Menopause which affects collagen turnover significantly. In these ‘less than optimal metabolic states’ there are increased inflammatory markers in the bloodstream, and tendons appear to be random collateral damage.
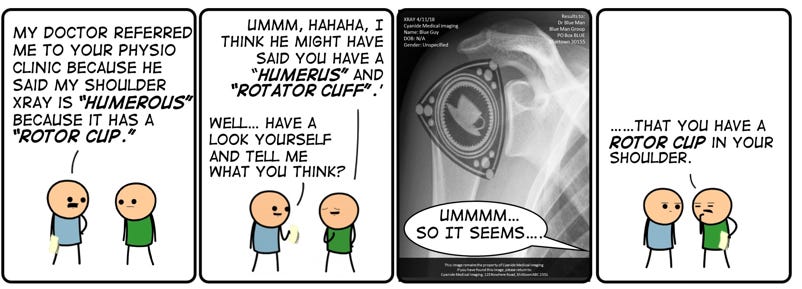
Even activity type plays a role and contributes to an ‘injury profile’: male walkers tend to get Achilles pain, female walkers get gluteal tendinopathy, yoga lovers get hamstring tendon pain from overstretching, and DIY home renovators doing lots of overhead tasks all of a sudden get rotator cuff issues (also lovingly known as ‘The Rotor Cup”).
We can almost place bets which tendon problem someone will develop based on their lifestyle.
Imaging: A Trap
One of my biggest frustrations? Unnecessary imaging. Patients with insidious onset tendinopathy don’t need ultrasounds or MRIs right out of the gate.
Imaging often leads to unnecessary worry and interventions. Unless we’re ruling out something sinister (fractures, space-occupying lesions, etc.), imaging should take a backseat. In fact, I’m yet to see imaging of a true Tennis Elbow do anything to guide management of a true case of Lateral Elbow Tendinopathy.
Before we end: STOP! Is it actually ‘Lateral Elbow tendinopathy’?
Misdiagnosing Tennis Elbow (Lateral Elbow Tendinopathy) is a common pitfall. Many cases of lateral elbow pain aren’t actually Tennis Elbow, they often are local or referral neurological pain (eg: radicular pain or ‘armatica’ as I call it), or even intra-articular (in the joint) elbow issues.
🔹 True Tennis Elbow = Localized pain over the lateral epicondyle, aggravated by gripping, particularly in pronation and elbow extension. Usually (but not always) a mechanical onset (doing too much/too soon gripping).
🔹 Not Tennis Elbow? = No pain at the lateral epicondyle. No difference in pain with gripping in neutral vs pronated/extended arm. For neck referred, usually came on gradually with prolonged sitting.
A thorough assessment is key. Treating the wrong condition means wasted time, ineffective rehab, and unnecessary frustration.
This is covered extensively in the previous blog.
And please, please, please:
“Tennis Elbow” is not an umbrella term for any pain in the elbow.
The Takeaway
Lateral elbow tendinopathy is frustrating — for patients and clinicians. The best approach? Accept the long recovery timeline, manage pain with patient-led strategies, and avoid falling for the ‘quick fix’ trap. As much as we’d love a miracle cure, the best thing we can do is coach patients toward managing their condition with realistic expectations and empowering strategies.
Who do I subscribe to for management techniques? I’m fans of Leane Bisset and Bill Vicenzinos work over the years.
Did this challenge your thinking or add value to your patient care? If so, even a small contribution helps me keep content like this going.
If this post helped you rethink an approach, refine a diagnosis, or improve patient outcomes, consider supporting my work.
☕ Buy Me a Coffee to say thanks, or become a paid subscriber—healthcare providers who subscribe can share cases with me or ask clinical questions anytime.
Tailor your Nick Ilic | Physio Clinician subscription:
You can customise which topics you receive updates for by selecting 'Manage Subscription' in your Substack options (in your browser), or by clicking 'unsubscribe' at the bottom of any email—don’t worry, it won’t unsubscribe you immediately! You'll then be able to choose your preferred sections:
✅ Patient Playbook
✅ Clinician’s Corner
✅ Research Reviews
✅ Clinician’s Compass
Choose what suits you best—I promise I won’t take it personally!