Patients Playbook | Understanding Osteoarthritis
More Than Just "Wear and Tear"
This post is an introductory preview—the valuable clinical insights, practical recommendations, and expert guidance are behind a paywall for paid subscribers only.
If you find my free content helpful, becoming a paid subscriber gives you:
✅ Full access to expert-backed strategies and pain management insights
✅ Direct access to me via subscriber chat—ask me questions anytime
✅ Ongoing, high-value information normally provided in a clinic for hundreds of dollars
This post is a guide only and should not be taken as medical advice. It does not replace assessment and recommendations from a registered and regulated healthcare professional.
The Big, Scary Label
Osteoarthritis (OA) carries an intimidating reputation. The moment patients hear it, they often imagine a one-way ticket to joint replacement surgery.
Patients worry about a lifetime of pain, and a future where playing with the grandkids or enjoying their favourite activities is off the table.
But this fear-driven narrative is outdated and, in many cases, flat-out wrong.
What Is Osteoarthritis Really?
Osteoarthritis (OA) is the world’s most annoying joint problem, affecting 1 in 4 people and making knees, hips, and other joints creak like an old door hinge. Keeping inflammation under control through exercise, diet, and lifestyle changes is the best way to keep your joints from going full rust-bucket mode.
Right now, science hasn’t found a way to stop it in its tracks, so researchers are on a mission to crack the code.
Metabolic Syndrome
One major culprit? Obesity-related metabolic syndrome—basically, when your body’s metabolism goes rogue and inflammation runs wild. But here’s the kicker: while it’s a huge risk factor for OA, it could also be preventable.
Scientists are still piecing together exactly how metabolic syndrome fuels OA, but the common denominator seems to be chronic, low-grade inflammation—the body’s equivalent of leaving the stove on just a little too long.
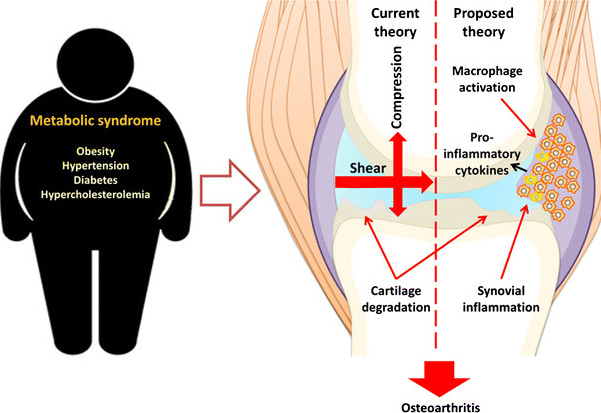
Immune cells (macrophages) in the joint lining (synovium) are like rowdy houseguests—once they show up inflamed, they don’t want to leave. This ongoing inflammation keeps the joints irritated, leading to more damage. Because of this, researchers are now eyeing these troublemakers as potential targets for new OA treatments—like bouncers kicking them out before they trash the place.
Bottom line: OA isn’t just about “wear and tear”—your immune system, metabolism, and inflammation are all in on the plot.
Here’s another crucial fact: OA is a clinical diagnosis, not a radiological one.
Why the X-Ray Diagnosis Can Be Misleading
Osteoarthritis is diagnosed based on symptoms, not scans.
X-rays may show age-related changes (“degeneration”) in the joint, but that doesn’t automatically mean the person has OA.
If we scanned every 70-year-old in Australia, plenty would have signs of OA on imaging but no symptoms. Or put another way—just because a house has a few cracks in the paint doesn’t mean it’s about to collapse.
A diagnosis usually requires matching those imaging findings with a patient’s symptoms and history. However, given that changes on X-ray don’t matter, X-Rays are not needed to diagnose Osteoarthritis.
Too often, patients are told they have OA based on an X-ray alone. This can lead to unnecessary anxiety, misguided treatment plans, and even premature surgeries.
I once had a patient scheduled for a knee replacement in two weeks, solely based on an X-ray. After a proper assessment, we found they had a simple, short-term joint issue. Within a week of proper management, their pain resolved, and surgery was cancelled—saving them time, money, and an unnecessary operation.
Moral of the story? Not every creaky door needs to be knocked down and rebuilt.
Don’t become a V.O.M.I.T. (Victim of Medical Imaging Technology).
Common Symptoms of OA
Knee and Hip OA symptoms follow a typical pattern:
Morning stiffness (~30mins to get going)
Pain after prolonged sitting (e.g., long drives or flights)
Aches later in the day
Occasionally, night pain, though sleep onset is usually fine
Hip OA in particular tends to cause functional issues like:
Difficulty putting on shoes and socks
Difficulty getting in and out of cars
and when it gets really bad: Difficulty getting off the Toilet (this hits the ego hard enough that it’s usually the final straw before seeing the Knee Replacement Doc).
Knees and hips also differ in how they develop OA.
Hip OA appears to run in the genes more than Knee OA, and is less often influenced by lifestyle and metabolic factors than knee OA.
This is why treating OA isn’t just about the joint—it’s about managing the whole person.
This is where our free subscribers leave us, and our paid subscribers get all the juicy and valuable information.
Keep reading with a 7-day free trial
Subscribe to Nick Ilic | Physio Clinician to keep reading this post and get 7 days of free access to the full post archives.