Patients Playbook | Why It Might Be Time to Talk Rheumatology
It’s Not All in Your Head—It Might Be in Your Immune System
This post is an introductory preview—the valuable clinical insights, practical recommendations, and expert guidance are behind a paywall for paid subscribers only.
If you find my free content helpful, becoming a paid subscriber gives you:
✅ Full access to expert-backed strategies and pain management insights
✅ Direct access to me via subscriber chat—ask me questions anytime
✅ Ongoing, high-value information normally provided in a clinic for hundreds of dollars
This post is a guide only and should not be taken as medical advice. It does not replace assessment and recommendations from a registered and regulated healthcare professional.
Sometimes someone comes in with pain in one area, and things just don’t add up.
As physios, we’re pretty good at figuring out what’s going on when a shoulder hurts, or a back flares up, or a tendon’s grumbling. But every now and then, we see something that doesn’t quite follow the usual script—pain in multiple areas, symptoms that don’t behave mechanically, or other signs that go well beyond joints and muscles.
That’s when we start thinking bigger picture. One of the most common areas of investigation? Rheumatology.
What is Rheumatology?
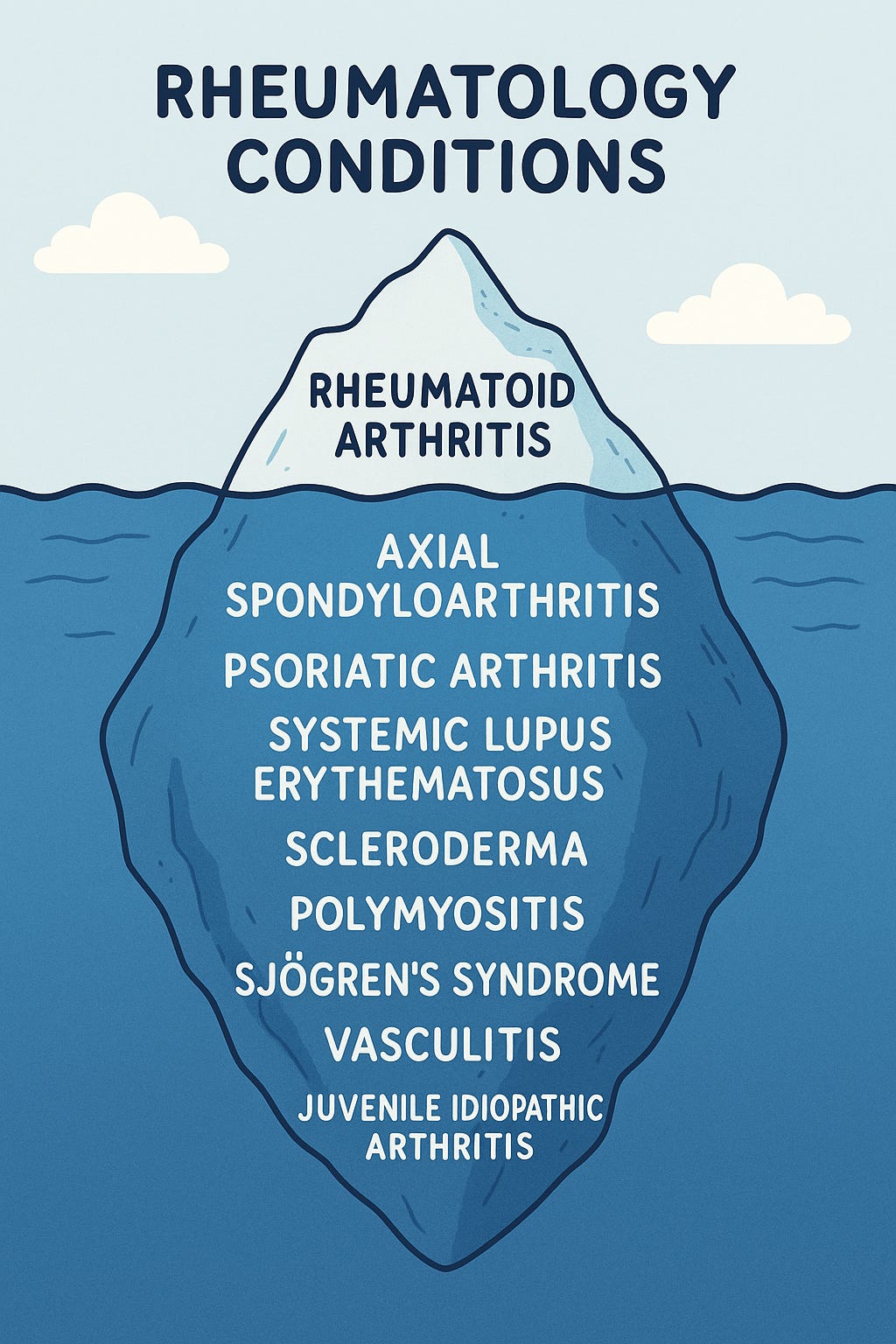
Rheumatology is the branch of medicine that deals with autoimmune conditions—when your immune system decides it’s time to go rogue and attack your own body. You’ve probably heard of rheumatoid arthritis—an autoimmune condition that targets small joints like the hands and feet. But rheumatoid arthritis is just the tip of the iceberg.
There’s a whole family of rheumatic diseases that can show up in different ways and at different stages of life. Some start during teenage years or early adulthood. Others tend to appear between the ages of 40 and 60. And here’s the kicker—if we catch them early, we can often slow them down or stop them from causing long-term damage.
But when they're missed or mislabelled as a local issue, they can quietly progress for years.
Why Are Rheumatic Diseases Hard to Diagnose?
Because they’re sneaky.
There’s no single test that definitively says “Yes! You have a rheumatic disease.” Instead, diagnosis is like building a jigsaw puzzle—except half the pieces are missing, and a few belong to a different puzzle entirely.
Here’s what we look at:
Blood tests (serology): These can check for markers of inflammation or specific antibodies (like rheumatoid factor, anti-CCP, or HLA-B27). But sometimes people with rheumatic disease have totally normal bloods. A negative (aka ‘sero-negative’) test doesn’t mean there’s nothing going on.
Imaging: MRI can show inflammation in joints and soft tissues, especially in conditions like axial spondyloarthritis (which affects the spine and pelvis). X-rays might not pick up anything until later stages. You can even have all the symptoms but clear imaging—this is known as non-radiographic axial spondyloarthritis.
There’s Rarely a Textbook Case
Here’s one of the biggest pitfalls: many patients don’t look like the textbook. And unfortunately, some GPs and clinicians will tell you exactly that—“You don’t fit the classic picture.” But the reality is, rheumatic diseases are messy. They evolve. They jump around. And they don’t follow neat rules.
Your symptoms still matter—even if they don’t come with textbook labels.
🔒 This section is for paid subscribers 🔒
Gain access to practical advice on what signs to look for, how to prepare for a rheumatology referral, and tips that help your clinicians help you sooner.
Upgrade to a paid subscription to keep reading.
Keep reading with a 7-day free trial
Subscribe to Nick Ilic | Physio Clinician to keep reading this post and get 7 days of free access to the full post archives.