Clinician’s Corner: Differentiating Hip Joint, SIJ, and Lumbar Spine Pain
When referred pain plays musical chairs, here’s how to spot who’s sitting where.
This blog is written for the clinician who’s halfway through a consult, already sensing that something doesn’t add up. The tests aren’t lining up. The symptoms feel familiar but don’t quite follow the script. And the more you prod, stretch, and ask, the more you realise: this isn’t about finding one magic test — it’s about building a case. We’re diving deep into the art (and science) of separating hip joint, SIJ, and lumbar spine drivers of pain. Not through textbook purity, but through clinical pattern recognition, contextual clues, and a ruthless suspicion of oversimplified labels. If you're here to sharpen your eye for the subtleties — welcome.
The first part of this post is an introductory preview—the valuable clinical insights, practical recommendations, and expert guidance are behind a paywall for paid subscribers only.
If you find my free content helpful, becoming a paid subscriber gives you:
✅ Full access to expert-backed strategies and pain management insights
✅ Direct access to me via subscriber chat—ask me questions anytime
✅ Ongoing, high-value information normally provided in a clinic for hundreds of dollars
This post is a guide only and should not be taken as medical advice. It does not replace assessment and recommendations from a registered and regulated healthcare professional.
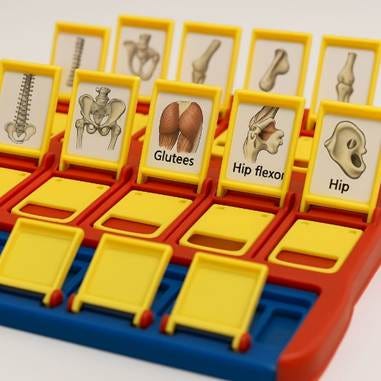
You’ve seen the patient: vague pain somewhere around the back, glute, groin, or thigh. The story’s a bit fuzzy. And you’re stuck toggling between lumbar spine, SIJ, and hip joint like you’re playing Guess Who with referral patterns.
This is the Bermuda Triangle of Musculoskeletal Healthcare.
They’ve probably already been labelled—tight hip flexors, twisted pelvis, non-specific back pain. Maybe even all three. Some walk in and thrust the GPs Lumbar Spine CT Scan in your face, and the referral to ‘try some physio’ for their age-related disc bulge (as they start pointing at their hip joint referred symptoms). But you know better: it’s your job to strip the noise, pick up the real pattern, and land the right diagnosis.
This blog isn’t a full deep dive into every possible cause of lumbopelvic pain. It’s a clinical walk-through to help you sort the big three suspects—the hip, the SIJ, and the lumbar spine—when they all start sounding the same.
At the very least, this blog will be helpful at making some connections in your mind and help you find the pattern you were looking for.
Pain in the lower back, buttock, and hip region often leads to diagnostic confusion, given the overlapping referral patterns of the Hip Joint, sacroiliac joint (SIJ), and Lumbar Spine. But if you've been in clinic for any length of time, you'll know there's usually a way to tease them apart—if you ask the right questions, listen properly, and test smart.
There’s so much overlap that site of pain alone doesn’t help—not without context.
Here’s a hot tip: Never trust what the patient is saying.
“WOAH NELLY! HOW DARE YOU!” I hear you say. Give me a second, and I’ll explain:
Don’t trust what they say—trust where they show you. Watch their hand. Ask them to point.
And listen to how vague they are. The patient is often apologetic about that vagueness, but I thank them for it: vagueness speaks volumes. Some pain sources are loud and specific. Others mumble.

If the story sounds fuzzy, it’s often because the joint talking to you has a broken microphone.
Despite being underseen - SIJs (Sacroiliac Joints) are often over diagnosed (especially by those obsessed with pelvic manipulation techniques). The Hip Joint? Often the most poorly recognised major joint—especially in younger non-OA cases. It’s the ‘middle child’ of MSK—ignored, misunderstood, and always trying to prove itself.
Quick Ratio Check (based on clinic experience in private Msk practice):
1 SIJ for every 18 hips for every 20 Lumbar Spines.
The key thing is, most of this is a matter of ruling out* as much as possible then trying to make the best of what’s left on your Guess Who board.
Specifically, during the physical examination: the Hip Joint is the easiest to rule out*, followed by the Lumbar Spine (for mechanical low back pain, not so much Spondyloarthropathies), and the SIJ is extremely difficult to rule out.
*OK, let’s pause for a reality check.
Throughout this blog I’m going to sound super dooper confident and say things like:
“Rule out” or “Rule in.”
Every time you see that, I want you to hit Ctrl+H in your brain.
Replace “Rule out” with: Consider much less likely.
Replace “Rule in” with: Consider much more likely.
That’s how clinical reasoning actually works—we’re dealing in probabilities, not absolutes.
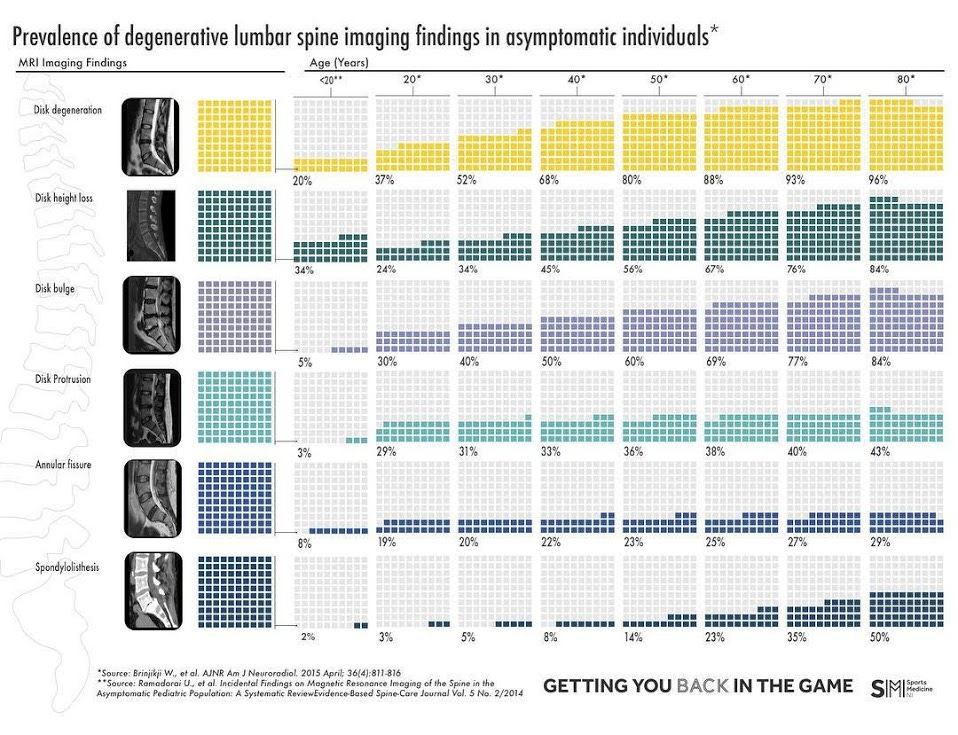
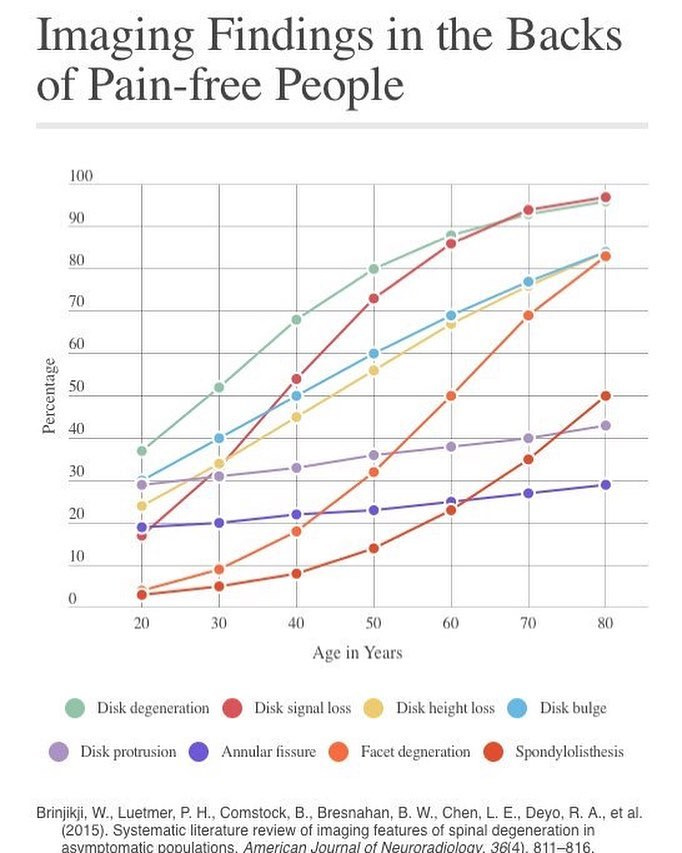
A Quick Word on Diagnostic Imaging
Those who rely on imaging alone for diagnosis are doomed to misdiagnose. Imaging should always be interpreted in the context of clinical assessment. "Degeneration"—radiology-speak for age-related changes—is everywhere, especially in people who, well... have aged.
There’s a Butt-tonne of Ass-ymptomatic people walking around with backsides that don’t look great on imaging. Here's the kicker: most of them feel fine.
In the lumbar spine: A systematic review by Brinjikji et al. (2015) found that signs like disc degeneration, disc bulges, and facet joint changes were seen in high percentages of asymptomatic people. For example, disc degeneration was found in 37% of 20-year-olds and up to 96% of those in their 80s. (Brinjikji et al., 2015)
In the SIJ: CT imaging showed sacroiliac joint degeneration in 65.1% of asymptomatic adults, with substantial degeneration in 30.5%—and 91% of those in their 80s. (Eno, Boone, Bellino, & Bishop, 2015)
In the hip: Studies show cam deformities in 37% and pincer deformities in 67% of asymptomatic individuals. That’s before you even touch on the incidental labral tears and signs of impingement in people with no symptoms. (Frank et al., 2015)
Imaging might show you a mess—but it doesn’t tell you what hurts. That’s your job.
So before you treat the scan, treat the person. Use your ears, hands, and brain. Because diagnosing from an image is like treating a shadow—you’ll always miss the mark.
Keep reading with a 7-day free trial
Subscribe to Nick Ilic | Physio Clinician to keep reading this post and get 7 days of free access to the full post archives.