Take-off to Touchdown | Chapter II | Management of The Older Shoulder
Management of Rotator Cuff related pain, Sub acromial Bursitis, and much more.
The first part of this post is an introductory preview—the valuable clinical insights, practical recommendations, and expert guidance are behind a paywall for paid subscribers only.
If you find my free content helpful, becoming a paid subscriber gives you:
✅ Full access to expert-backed strategies and pain management insights
✅ Direct access to me via subscriber chat—ask me questions anytime
✅ Ongoing, high-value information normally provided in a clinic for hundreds of dollars
This post is a guide only and should not be taken as medical advice. It does not replace assessment and recommendations from a registered and regulated healthcare professional.
The Series:
(You are here) Chapter II | The Older Shoulder
Take-Off
Ensure you have completed all pre-flight checks, all patient baggage has been checked in and stowed, patients have been through all checkpoints, and have been thoroughly screened to ensure they are on the right flight.
Triage for Red Flags and Urgent Referrals

If insidious/low force onset:
Continue without imaging initially for Musculoskeletal (MSK) presentations.
See a MSK clinician with a minimum of 45 minutes for the initial appointment.
XR if ruling out medical red flags.
GPs should refer to a reliable physiotherapist for low-cost/high-value care.
If high force trauma history:
Immediate XR (usually done in ED/A&E) if severe pain or loss of glenohumeral joint (GHJ) function.
Follow up CT if fractures on XR and surgical referral is likely (most likely referred by orthopaedic specialist).
MRI if no improvement in GHJ function and pain despite rehab at weeks 6-8.
Patient History/Profile
Classify the Patient into a Cohort:
To aid short-list of likely differential diagnoses.
Paediatric patients and young adults get different insidious onset and traumatic GHJ pathology than middle aged and older adults.
Females 50-60yrs are more likely to develop adhesive capsulitis.
Patients > 75-80yrs are less likely to have primary rotator cuff referred pain if it its their first presentation - check cervical spine.
Inflammatory profile and metabolic status: Consider medical status (diabetes, obesity, smoker, menopause, auto-immune inflammatory diseases etc.)
Psychosocial profile: Check for nocebic beliefs, especially those influenced by past healthcare providers and radiology, family history, patient goals, occupation, etc.
Current medications: Review the list for unreported medical history.
Previous prescription of oral NSAIDs: Assess tolerance and side-effects.
Previous imaging and procedures: Review past imaging to rule out significant issues and check for effectiveness of recent US guided HCLA injections for Bursitis.
Patient History
Mechanism of Injury: Hunt for the exact mechanism of injury. If insidious onset, query the 1-2 weeks in the lead-up to the pain
Injury History: Have they had this before? What made it better/worse, what was the duration of symptoms back then?
Pain Patterns for Differential Diagnostics:
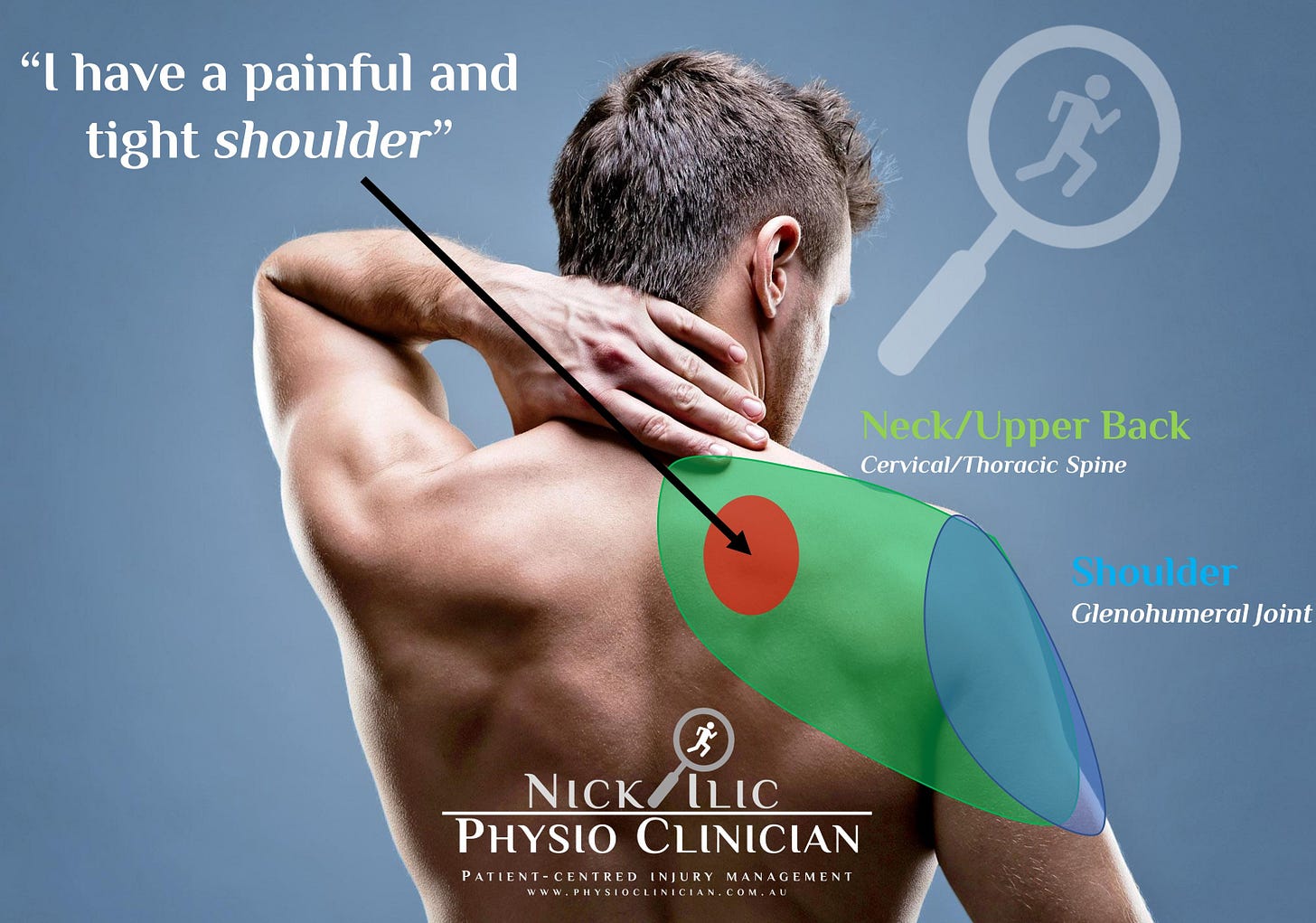
Location Map out exact pain referral patterns “point with your finger where your pain is” – pain past elbow, or pain into shoulder blade less likely to be Glenohumeral Joint.
Irritability/Severity – Mild/Moderate/Severe – speaks to the sensitivity of different structures
Pain Onset - Mechanical onset when using shoulder, or is it an achy pain after upper limb tasks.
Daily Pattern - Is there pain at night and in what positions (or is it any position?)
Top 3 painful tasks/activities – Track the top 3 things that bother the patient. (Utilise the PFPS formally or use it as a guide for tracking)
Physical Examination
Clear Cervical Spine as Cause/Contributor:
Glenohumeral joint and Cervical Spine are both relatively easy to rule out with good assessment.
Pain location (knowing what refers where) helps significantly here.
Bilaterality (pain on both sides) usually suggests Cervical Spine referral moreso than both GHJs.
Cervical Spine Cluster test: Upper Limb Neural Tension Tests, Spurlings Test, Specific Palpation of cervical column.
If suspected, utilise Neck and Low Back Pain Checklist
Rule out Adhesive Capsulitis/Frozen Shoulder – pain > stiff phase or stiff > pain phse. Loss of ROM in >2 directions and highly irritable.
Clear Other Shoulder Joints – Acromioclavicular Joint (ACJ) and Sternoclavicular Joint (SCJ)
Medical causes for pain: Obtain a solid medical history to rule out visceral pain referral and other medical causes (infections, neoplasms, insufficiency fractures).
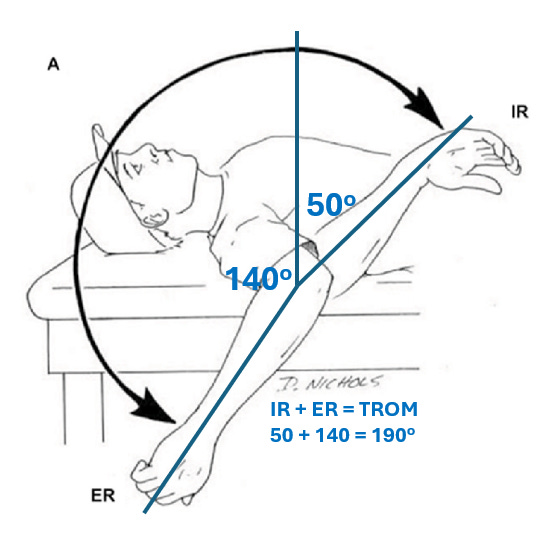
ROM, Strength and Functional Capacity Testing
AROM: Flexion, Abduction, External Rotation, Internal Rotation
PROM past the first point of AROM pain to rule out contractile tissue pain inputs.
A significant restriction in 2 or more ROM directions, particularly ER would suggest frozen shoulder or another significant ROM restricting pathology.
IR+ER ROM (Total ROM (TROM)) in Supine
Observation – for loss of muscle bulk (eg: infraspinatus muscle), check for pop-eye sign (bicep bunching), observe quality of ROM movement
Isometric Strength – utilising fixed or handheld dynamometry
External Rotation (0deg abduction) (ER0)
Internal Rotation (0deg abduction) (IR0)
External Rotation (90deg abduction) (ER90) - If ROM >110deg and patient usually active above shoulder height with gym, exercise, sports, ADLs, and/ or occupation.
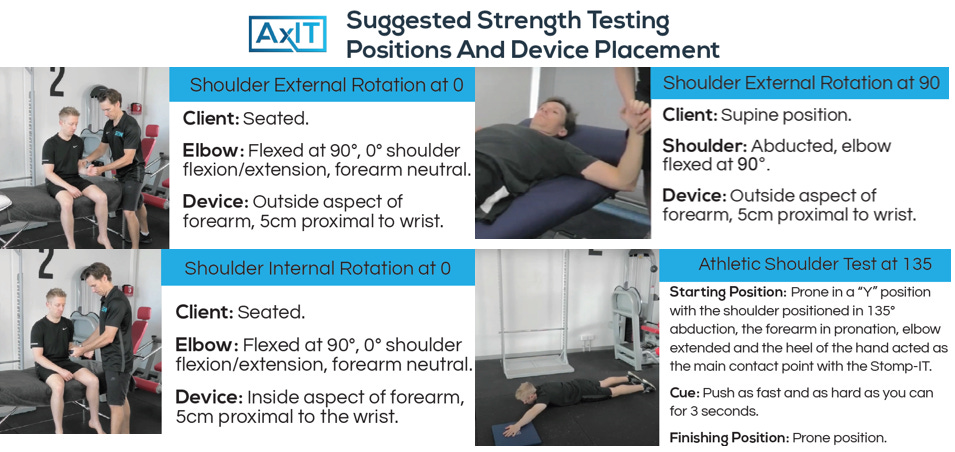
If good enough strength with IR0/ER0 and pain-free ROM > 135, consider ASH Test on force plates, fixed dynamometry or simple bathroom scales.
Apprehension test in upright position or supine if instability is suspected (less likely in the older shoulder)

Palpation
Cervical spine (Csp): Palpation is reliably sensitive but not specific (can be painful in asymptomatic patients), but absence of pain on palpation usually makes cervical spine issues less likely. There is a skill to correctly palpating the cervical spine with the patient in supine and head turned away, find an experienced practitioner to show you how.
Shoulder: Palpation of GHJ is unreliable (doesn’t rule in or out), not sensitive and not specific. Palpation of ACJ and SCJ reliably specific and sensitive (easy to rule out with palpation). Palpation of long-head biceps tendon (LHB) is unreliable for specificity, but reliable for sensitivity (absence of pain in bicipital groove makes LHB pathology less likely – if LBH is still there).
Diagnostic Labels to help guide management:
Pain levels: Label as mild/moderate/severe; avoid dwelling on VRS (“1-10 scale”).
If Cervical Spine involved, see Diagnostic Labels in Neck/Low Back checklist
Rotator Cuff Referred Pain for weak and painful shoulders.
Shoulder Instability for unstable and painful shoulders.

🔒This is where the free preview ends. Paid subscribers now get access to the full post, including the clinical pearls, key takeaways, and practical recommendations.
Keep reading with a 7-day free trial
Subscribe to Nick Ilic | Physio Clinician to keep reading this post and get 7 days of free access to the full post archives.