Clinician's Compass | Staying in Our Lanes, Driving the Same Road
A physio’s reflection on mutual respect, better referrals, and when surgeons start handing out exercise sheets.
We’re all driving toward the same goal: better patient outcomes.
But when surgeons start prescribing rehab protocols without assessment—or physios send vague referrals—it’s time to talk lanes, scope, and mutual respect.A practical guide to collaboration (with a few A4-sheet war stories along the way).
This is a no-paywall blog post with insights I believe are valuable. If you find it useful, subscribe to my Substack for more in-depth content, exclusive case studies, and clinical insights.
Your support helps me continue sharing everything I’ve learned in the clinic with the world.
☕ Prefer a one-off thank you? Buy Me a Coffee.
The A4 Sheet Moment
It’s always a bit of a moment when a patient walks in clutching an A4 sheet of exercises from a previous healthcare provider – usually dated, often generic, and sometimes mildly tragic.
It’s even more of a moment when you realise it’s come from a well-meaning Surgeon who, for all their brilliance in the operating theatre, has just waded into your lane with the clinical equivalent of a 1999 glute bridge printout. Or the 2020s version, a public facing website with a series of recipes for various conditions.

We’d normally carefully prescribe specific exercises for the particular patient in front of us based on a thorough assessment (often with fancy gear like dynamometry), often just 2-3 exercises done well - especially for the busy 40yrs+ cohort.
So you know why we’re dazed and confused (just like the patients) when we see they’ve been given something like the below handout (or encyclopaedia), without assessment, and without a planned review to reassess how they’re going:
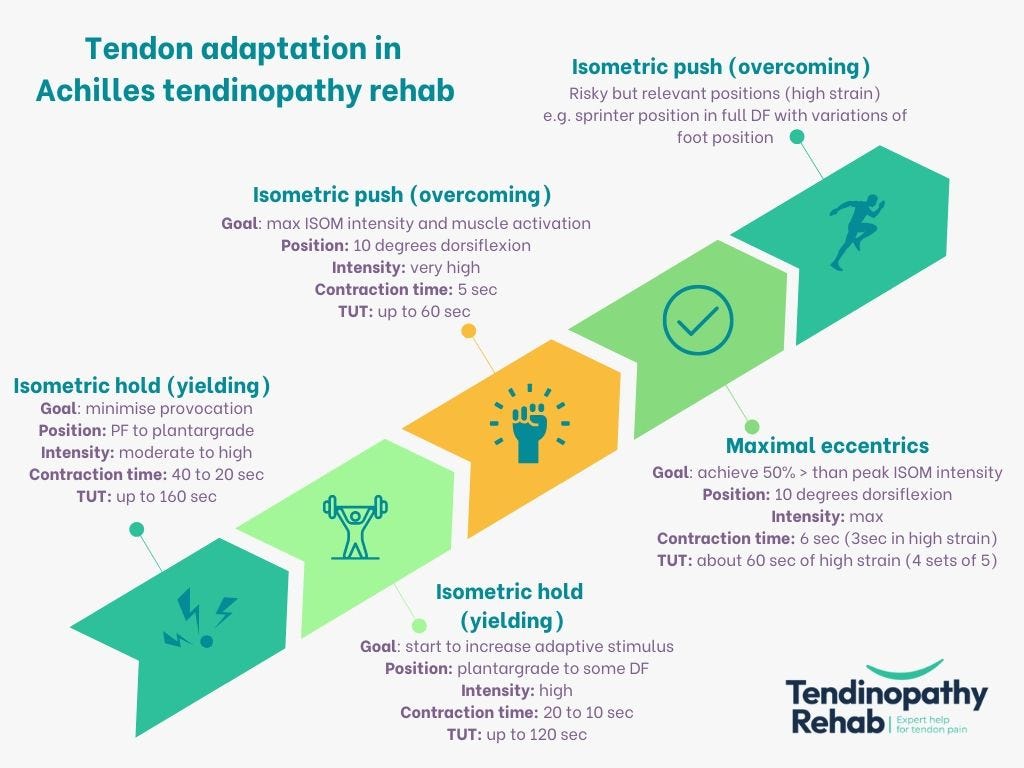
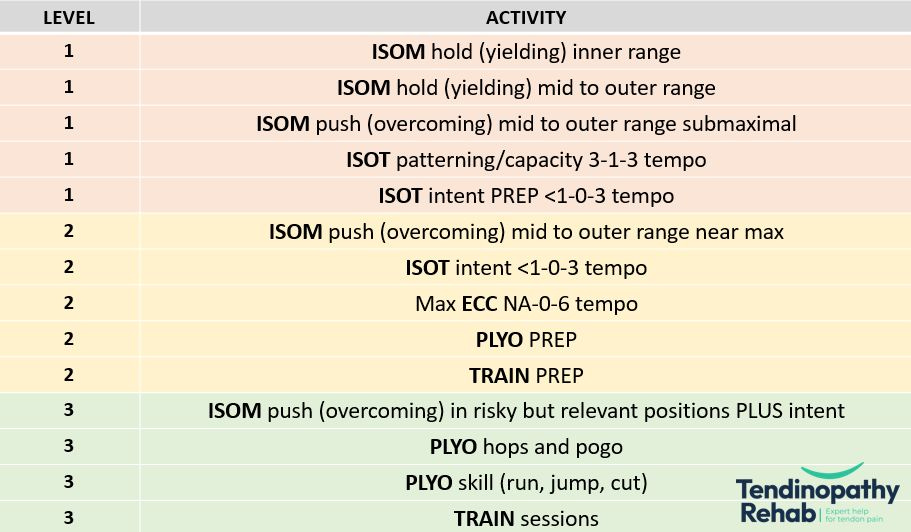
I recently spent an entire on a weekend course on lower limb tendinopathy. Predominantly for Achilles and Patellar Tendinopathy, it was a masterclass on the dark arts of assessing and prescribing tendon targeted interventions (or “exercises”) for these tendons.
Just so you understand the complexity, here’s the overview of just one of many frameworks on how to manage Tendinopathy.
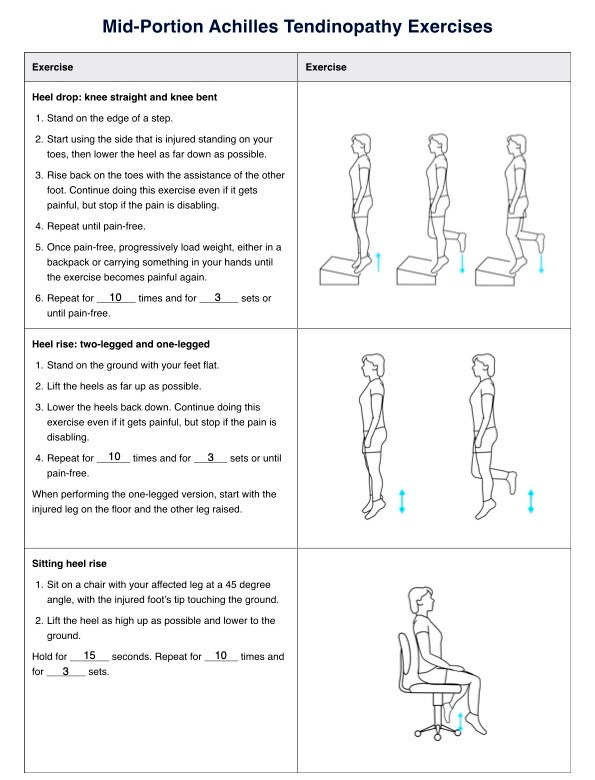
But if an athletic Achilles Tendon somehow made it’s way into a Physicians room, they might walk away with the following on a dusty A4 sheet:
I once had an entire room of GPs try to outdo each other in front of me to demonstrate their best Tennis Elbow can of beans exercise that fixes all of their elbow patients (or at least allegedly so - they rarely follow up because “it’ll go away in a year”). That memory will forever a bit of a giggle for me given the complexity in managing that condition.
Now, let me be clear: this isn’t a Doctor-bashing blog. Many of the GPs and Orthopaedic Specialists I know are absolute legends – collegial, curious, and fantastic at what they do. Their surgical expertise is world-class, and the volume of procedures they need to perform each year to maintain competence is staggering. A dedicated ACL surgeon who does multiple reconstructions per week will, of course, be sharper in that space than a generalist who dabbles. That’s expected.

So let’s flip the mirror: when it comes to conservative management of musculoskeletal conditions – assessment, diagnosis, rehab planning, and progression – I’ve simply done more reps. It’s what I live and breathe. I’ve spent years refining these skills, obsessively staying on top of the evidence, and managing these conditions every week. I’m not offended when a surgeon hands out an exercise sheet with extremely outdated and incorrect information; I’m just quietly amused. Because that’s not really their jam. And that’s okay.
Different Lanes, Same Road
The better metaphor isn’t turf war, it’s traffic: we’re driving in parallel lanes, heading to the same destination. We want the patient to get better.
We want them to avoid unnecessary interventions and, when needed, we want them to get the right one. But just like you wouldn’t want your Exercise Physiologist triaging you for a fresh traumatic knee instability injury, it’s probably not ideal for a surgeon or a GP, or even a Sports Physician to manage the nuanced, non-surgical pathway of a complex tendinopathy.
Why It Happens
Well, for starters, the Doctor might just be trying to help.
The patient could’ve been referred directly by a GP, or the physio referral might’ve been vague or non-existent. Maybe the surgeon doesn’t know there’s a competent rehab clinician involved. Or maybe their past experiences with rehab have been disappointing.
Let’s face it: if all they see are failed rehab attempts, they’ll assume most rehab isn’t great.
That’s the survivorship bias problem.
Surgeons rarely get to see the wins. They don’t see the meniscus injuries that never needed surgery, the labral tears that settled, the wobbly shoulders that unwobblefied themselves following months of solid rehab.
They see the breakdowns, not the breakthroughs.
Making a Good Referral Great
None of this is fixed by finger-pointing. The responsibility lies with all of us. Physios and rehab clinicians, should write good referrals. Show your working - tell the story, discuss your clinical reasoning. Don’t just say "failed rehab, please assess and advise."
Tell the surgeon what you’ve tried, why you’re referring, what you’re hoping for, and what your plan would be.
That context is gold.
It lets the surgeon back you, and helps the patient hear a unified message.
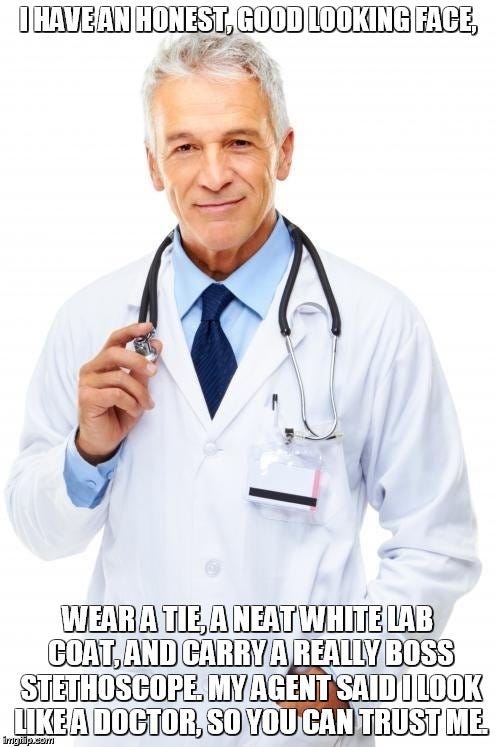
The Illusion of Authority
Doctors still carry a kind of inherited cultural clout.
Patients trust the white coat and the competence . And honestly, who can blame them? It’s a compelling image: the decisive doctor, sweeping in to save the day with clarity and confidence. But here’s the rub (from a glorified massage therapist, no less):
At our local uni, medical students get a few short months of MSK (musculoskeletal) training - if that.
We spend 4–5 years studying it, then build careers specialising in it, and still squeeze in hundreds of CPD hours a year to stay sharp. Yet somehow, we’re still playing second fiddle in some patients eyes - and funnily enough, in some GPs eyes too.
Some Doctors think we’re an item on the shelf: “Oh well, that didn’t work, how about you try some Physio”.
Driving Forward – Together
At the end of the day, we’re not adversaries.
We’re professionals trying to get patients better.
We stay in our lanes, yes – but we drive the same road.
And when we do it well, the patient doesn’t even notice the handover.
They just feel like they’re getting where they need to go.
Did this challenge your thinking or add value to your patient care? If so, even a small contribution helps me keep content like this going.
If this post helped you rethink an approach, refine a diagnosis, or improve patient outcomes, consider supporting my work.
☕ Buy Me a Coffee to say thanks, or become a paid subscriber—healthcare providers who subscribe can share cases with me or ask clinical questions anytime.
Tailor your Nick Ilic | Physio Clinician subscription:
You can customise which topics you receive updates for by selecting 'Manage Subscription' in your Substack options (in your browser), or by clicking 'unsubscribe' at the bottom of any email—don’t worry, it won’t unsubscribe you immediately! You'll then be able to choose your preferred sections:
✅ Patient Playbook
✅ Clinician’s Corner
✅ Research Reviews
✅ Clinician’s Compass
Choose what suits you best—I promise I won’t take it personally!












I love this analogy, after being told to ‘stay in my lane’ by a psychologist- my reply was, we’re all driving on the same highway to the same destination and if I’m not changing lanes occasionally and talking to other drivers then it’s going to cause an accident!